If you’re relying on nasal or throat-based tests to give you a clean bill of health after a COVID-19 infection, you might be swabbing the wrong end.
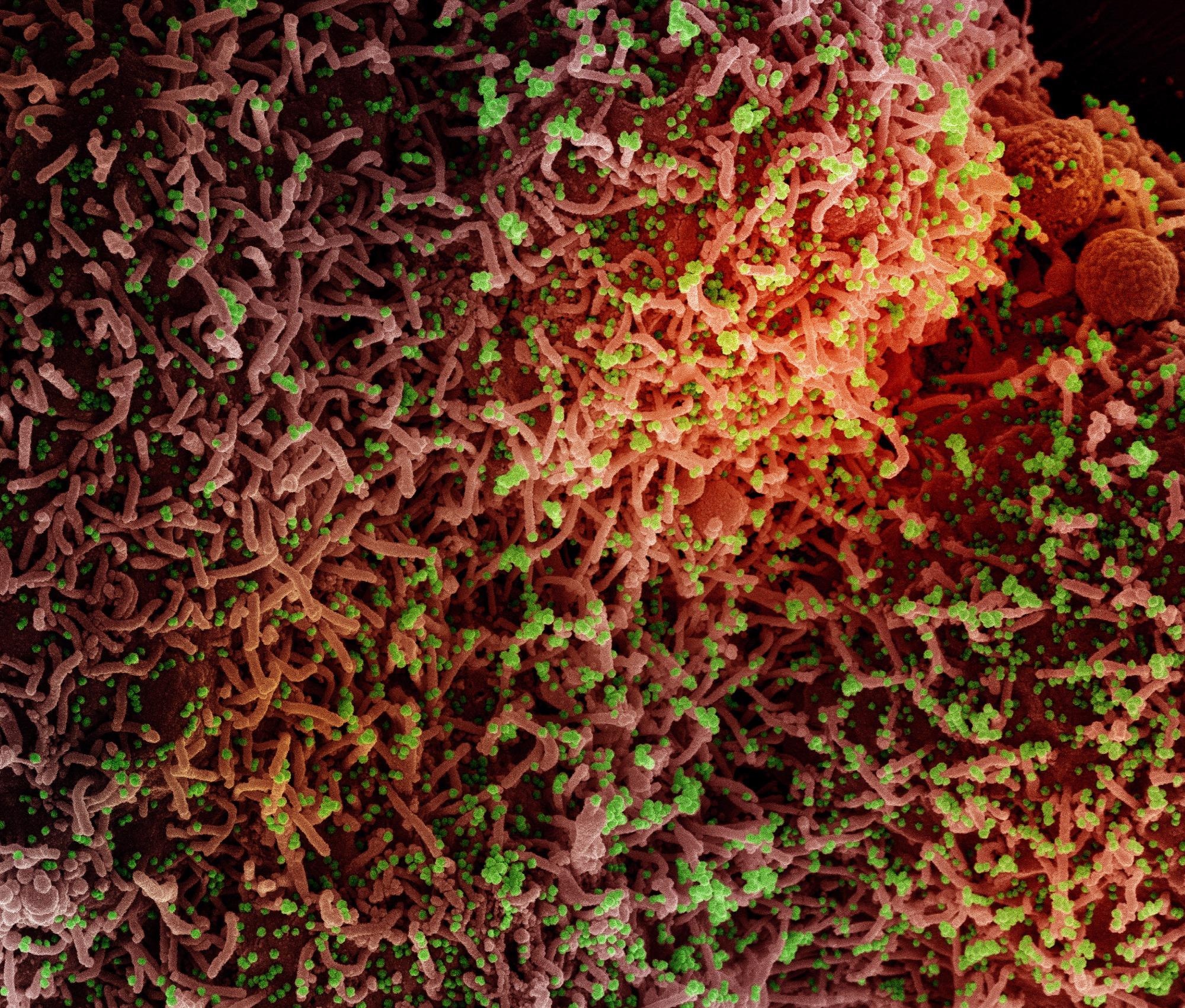 Study: Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Image Credit: NIAID
Study: Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Image Credit: NIAID
The study is the first to assess the presence of viral RNA in fecal samples from individuals with mild to moderate COVID-19 that are collected at various points after they became ill. It adds to mounting evidence that the SARS-CoV-2 virus actively infects the gut.
The findings don’t imply that there is fecal-to-oral transmission of the virus that causes COVID-19, the researchers caution. They were isolating fragmented genetic material rather than intact, infectious viral particles. But the results highlight a possible viral reservoir that could partially explain the mystifying constellation of symptoms that plague a minority of COVID-19 patients for months after their initial infection.
“No one really knows what causes long COVID,” said Ami Bhatt, MD, Ph.D., associate professor of medicine and of genetics. “But our study shows that SARS-CoV-2 can hide out in the gut for months. Maybe long COVID — and the wide variety of symptoms it causes — is due to the immune system’s response to viral proteins in hidden reservoirs throughout the body.”
COVID and the microbiome
People with primarily gastrointestinal symptoms could have a persistent viral infection in their intestines, for example. Others with the mental confusion commonly called “brain fog” could similarly have a lingering infection in their nervous system, Bhatt speculated.
Bhatt is the senior author of the study, which was published online in the journal Med on April 12. Postdoctoral scholar Aravind Natarajan, Ph.D.; research scientist Soumaya Zlitni; laboratory manager Erin Brooks; and research scientist Summer Vance are the lead authors of the study.
Bhatt, who researches how the microbiome — the vast universe of bacteria that carpets the lining of our intestines — affects human health, is eager to study whether an individual’s bacterial “gutprint” affects whether, how and for how long the virus is shed in their feces after infection with SARS-CoV-2. She and her colleagues are continuing their study of viral shedding in fecal samples as part of the nationwide RECOVER Initiative sponsored by the National Institutes of Health.
The research team took advantage of an early clinical trial launched in May 2020 at Stanford Medicine of a possible treatment, interferon lambda, for mild COVID-19 infection. Participants in the trial were monitored to follow the evolution of their symptoms and the degree and location of viral shedding. Fecal samples were collected from participants at specific time points as part of the trial.
The researchers piggybacked onto the interferon lambda trial because the participants were less sick than the hospitalized patients who were the focus of many other investigations at the time. They wanted to track what was happening in the majority of patients — those with mild illness.
Bhatt and her colleagues analyzed samples from 113 people at different points after infection. They found that about half of the people with mild to moderate cases of COVID-19 were shedding viral genetic material in their feces within a week after they tested positive for the SARS-CoV-2 virus. About 13% of people were still shedding viral RNA four months later after they had cleared the virus from their airways, and nearly 4% had viral RNA in their feces seven months after their initial infection.
Fecal shedding also correlated with ongoing gastrointestinal symptoms of the virus, including nausea, vomiting, and abdominal pain.
“It’s not clear why some infected people have GI symptoms,” Bhatt said. “But other coronaviruses are known to infect the gut in animals, so the idea of ongoing infection is not far-fetched.”
The researchers were not able to isolate enough viral RNA to determine which viral variant had infected the participants or to conclusively show that the samples isolated from any given individual at early and later time points were the same strain. But because the samples were collected relatively early in the pandemic, reinfection with a second strain or variant during the study was probably unlikely, the researchers believe.
Questions about wastewater
The findings have implications for the wastewater surveillance that researchers and governments are using to infer COVID-19 case counts in cities and counties around the country.
“We’re clearly seeing large and increasing amounts of the omicron subvariant BA.2 in wastewater nationwide,” Bhatt said. “At the same time, there have been lay reports that omicron is more likely than previous variants to cause GI symptoms. So, is this wastewater increase really proportional to the number of people who are infected? Or are more people shedding the virus in their feces for longer?”
Understanding the dynamics of infection and viral shedding is critical to planning, Bhatt argued.
“It’s hard to interpret wastewater surveillance if we don’t understand the biology that determines who is shedding, when and how much,” she said. “Early in the pandemic, many clinicians decided SARS-CoV-2 didn’t infect the gut, and that was dangerous to our understanding.”
The research was supported by the American Association for Cancer Research, the National Science Foundation, and the National Institutes of Health (grants R01 AI148623, R01 AI143757, and UL1TR003142), a Stanford ChemH-IMA grant, and a Stanford Dean’s Postdoctoral Fellowship.
Other Stanford authors are senior biostatistician Alex Dahlen, Ph.D.; Haley Hedlin, Ph.D., associate director of the clinical trials program, quantitative sciences; undergraduate student Ryan Park; graduate students Alvin Han and Danica Schmidtke; postdoctoral scholars Renu Verma, Ph.D., and Karen Jacobson, MD; Julie Parsonnet, MD, professor of medicine and of epidemiology and population health; Hector Bonilla, MD, clinical associate professor of infectious diseases; Upinder Singh, MD, professor of medicine and of microbiology and immunology; Benjamin Pinsky, MD, Ph.D., associate professor of pathology and of medicine; Jason Andrews, MD, associate professor of medicine; and Prasanna Jagannathan, MD, assistant professor of medicine.