The motile cilia that line the epithelial tissue of the airways are considered the first line of defense against pathogens that cause several respiratory diseases. The airway epithelium consists of one to two hundred cilia at their surface that primarily secrete viscoelastic mucus, which helps to trap inhaled particles, including viruses.
The particles that are trapped within mucus are then brought towards the pharynx through the coordinated beating of cilia, which subsequently allows for the mucus to be swallowed or expelled.
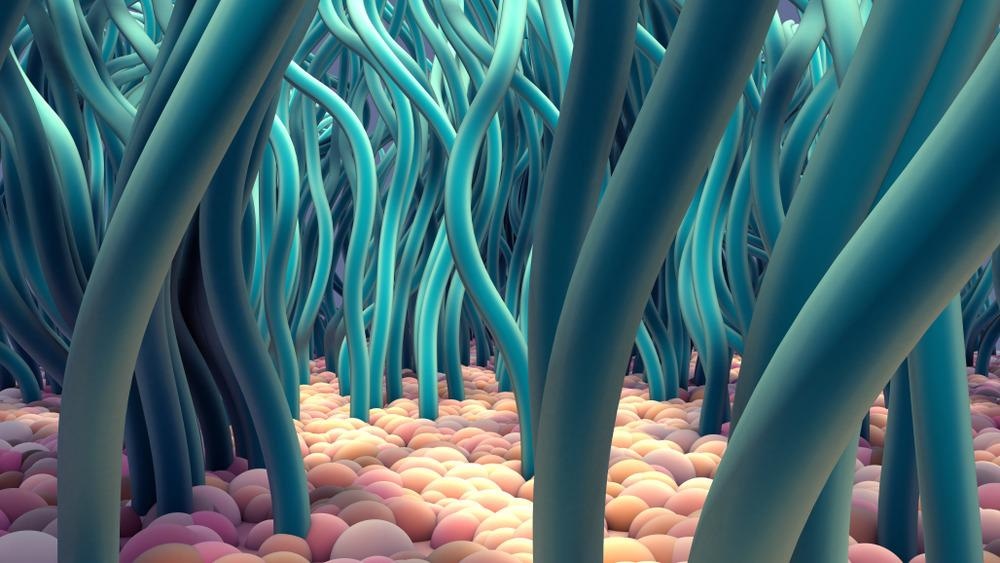
Study: A close shave: How SARS-CoV-2 induces the loss of cilia. Image Credit: Design_Cells / Shutterstock.com
Background
Several respiratory pathogens have developed different mechanisms to escape the mucociliary clearance pathway. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), for example, appears to directly infect ciliated cells and destroy cilia.
Previous studies have identified the SARS-CoV-2 open reading frame 10 (ORF10) protein to be responsible for the loss of cilia as a result of its role in promoting the ubiquitin-dependent degradation of ciliary proteins.
To this end, the SARS-CoV-2 ORF10 appears to interact with the E3 ubiquitin ligase adapter ZYG11B. E3 ubiquitin ligases also interact with E2 ubiquitin-conjugating enzymes and E1 ubiquitin-activating enzymes to attach to ubiquitin and target proteins. Notably, many viruses have evolved mechanisms to escape the ubiquitin/proteasome pathway by encoding E3 mimic proteins that aid in the degradation of antiviral cellular proteins.
In a new Journal of Cell Biology study, researchers aimed to determine whether the interaction between ORF10 and ZYG11B promotes the dissemination of SARS-CoV-2.
About the study
The current study involved pull-down experiments to confirm the interaction between the SARS-CoV-2 ORF10 and ZYG11B. Tandem Mass Tag (TMT) proteomics analysis was used to determine the effect of ORF10 on the cellular proteome, followed by Western blot analysis. The dose-dependency of the ORF10 effect was also evaluated.
In vivo studies involving human angiotensin-converting enzyme 2 (ACE2) knock-in mice were also conducted using a lentiviral vector carrying ORF10 to better understand the role of this viral protein during SARS-CoV-2 infection.
Study findings
The in vitro interaction between the SARS-CoV-2 ORF10 and ZYG11B led to increased ubiquitination activity in the presence of specific E1 and E2 enzymes.
Expression of ORF10 also caused the downregulation of 352 proteins, while only two proteins were upregulated. Most of the downregulated proteins were found to play a role in the biogenesis, structure, and maintenance of cilia. Some of these proteins included TALPID3, TTBK2, BBS4, SEPTIN2, and IFT46.
The dose-dependency studies on ORF10 revealed that higher expression of this viral protein had a greater impact on the downregulation of the aforementioned cilia proteins.
Several experiments were conducted on serum-starved transformed cell lines to inhibit the cellular division and allow for the formation of primary cilia. ORF10 transfection, both before and after starvation, reduced the number of cells that carried primary cilium. Taken together, these experiments similarly confirmed that ORF10 inhibits the biogenesis and maintenance of cilia. Notably, the knock-down of ZYG11B inhibited this activity of ORF10.
The expression of ORF10 was found to significantly downregulate the ciliary Intraflagellar Transport 46 (IFT46) protein. Increased expression of IFT46 rescued ciliogenesis in cells that overexpressed ORF10, thus demonstrating that the degradation protein of this protein is involved in the mechanism by which ORF10 alters ciliogenesis.
However, when the IFT46 protein lacking the C2 domain was overexpressed in ORF10-expressing cells, cilia biogenesis was partially recovered. This finding indicates that a completely functional IFT46 protein is not necessarily needed for cilium recovery during SARS-CoV-2 infection.
The in vivo lentiviral vector transfer of ORF10 to mice indicated that transferred ORF10 could lead to a loss of cilia within the epithelial cells that line the trachea. Notably, when mice were pseudotyped with the SARS-CoV-2 spike protein alone, this effect on the cilia was not observed, thus demonstrating that the SARS-CoV-2 spike protein is not capable of damaging cilia alone.
Conclusions
SARS-CoV-2 targets the ubiquitin/proteasome pathway and subsequently leads to the loss of ciliary proteins. More specifically, the SARS-CoV-2 ORF10 protein is responsible for the degradation of various ciliary proteins that ultimately reduce viral particle clearance and allow for the continued spread of SARS-CoV-2 throughout the respiratory tract.
Journal reference:
- Fonseca, B. F. & Chakrabarti, L. A. (2022). A close shave: How SARS-CoV-2 induces the loss of cilia. Journal of Cell Biology 221(7). doi:10.1083/jcb.202206023.