Age and sex have been identified as important indicators of immunity to infectious diseases as well as vaccinations throughout the lifetime of an individual. According to some reports, women's immune systems are stronger than men's. A higher level of inflammation has been reported in older individuals due to impaired immune function. The impact of interactions between sex and age can be observed through clinical manifestations and epidemiology of respiratory infections such as COVID-19 and influenza.
Both COVID-19 and influenza comprise the largest population of diseases that can be prevented by vaccines and occur in older individuals. However, despite high vaccine coverage against seasonal influenza, approximately 4 million cases occur in older individuals annually in the United States, leading to 90 percent of influenza-related deaths. Furthermore, it has been reported globally that males experience a higher risk of influenza infection, hospitalization, and mortality with old age. A similar observation was made in the case of COVID-19, where males suffered from severe disease with old age.
Vaccines help to prevent mortality and morbidity associated with influenza and COVID-19 in older individuals. However, the impact of age and sex on vaccine responses is not thoroughly analyzed.
A review published in Frontiers in Aging analyzed the sex differences in the safety, effectiveness, and immunogenicity of influenza and COVID-19 vaccines in older individuals. It also analyzed the way sex brings about the modification of the impact of age-related factors on vaccination.
 Study: Roadmap for Sex-Responsive Influenza and COVID-19 Vaccine Research in Older Adults. Image Credit: Rost9 / Shutterstock
Study: Roadmap for Sex-Responsive Influenza and COVID-19 Vaccine Research in Older Adults. Image Credit: Rost9 / Shutterstock
Sex differences following influenza vaccination in older individuals
Previous studies have highlighted that older females vaccinated with several types of inactivated influenza vaccines (IIV) have higher influenza-specific memory B cells, post-vaccination antibody titers, specific memory B cells, rates of seroconversion, fold-rises in titers, and rates of seropositivity. Additionally, for high-dose IIV that contains four times the antigen compared to the standard dose, older females have shown a higher rate of seroconversion and post-vaccination titers than older males.
Sex differences concerning vaccine effectiveness (VE) have also been observed in older individuals. Previous research has reported VE to be higher among older females than older males across seven influenza seasons. Also, older females were found to report more adverse events (AE) compared to older males for both high and standard vaccine doses.
Sex differences following COVID-19 vaccination in older individuals
For COVID-19 mRNA vaccines, female long-term care facility residents (LTCFR) were reported to have more significant functional antibodies and IgG titers as compared to males following the first dose of vaccine but not after the second dose. Among recovered LTCFR, higher antibody levels have been observed in females compared to males. However, the sex differences concerning immunogenicity as well as vaccine effectiveness (VE) among older individuals who have received the mRNA vaccines are not entirely evident yet.
Few studies on COVID-19 vaccine safety have reported that systemic, local, and medically attended AE are more common among older females compared to older males. Older individuals have also been found to report lower AE as compared to younger individuals.
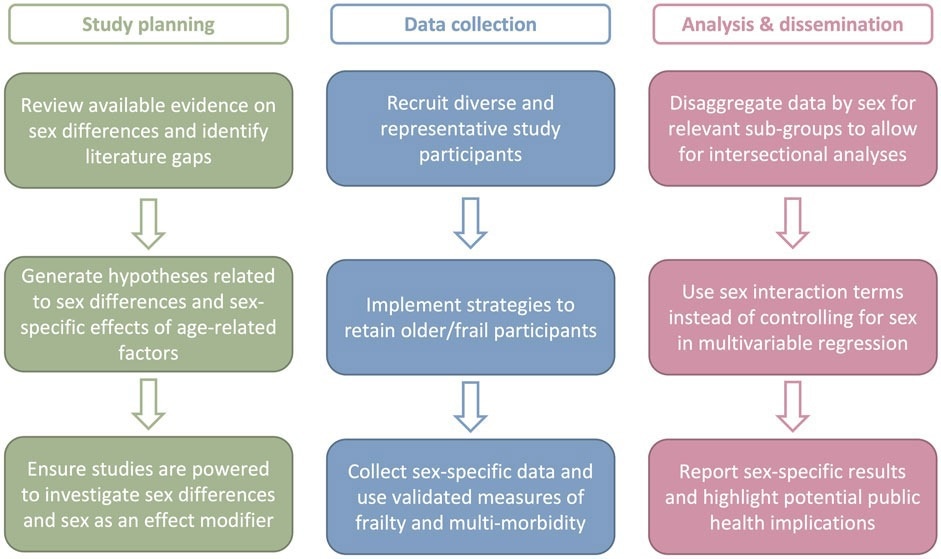
Roadmap for sex-responsive vaccinology research in older adults. Sex-responsive vaccine research in older adults requires careful thought and at the study planning, data collection, analysis, and dissemination phases. Action items for each phase are provided.
The intersection of age and sex
Age-related changes in immunity are observed to be accompanied by changes in the hormonal environment for both females and males, thereby leading to a sex-specific impact on aging. Moreover, a decrease in naïve T cell activity along with an increase in monocyte function with age has been observed more extensively in males as compared to females. This is further associated with a male-specific decrease in B cell transcriptional activity.
Furthermore, older females have been reported to enter each season of influenza with greater immunity compared to older males with high-dose IIV. However, for the pH1N1 vaccine, a decline in immunogenicity with age was observed in older females but not older males. For COVID-19 vaccines, studies on the VE and antibody response have indicated old age as a risk factor, but the sex-specific effects of aging have not been analyzed.
The intersection of frailty and sex
Frailty can be defined as a decrease in physiological function that leads to an increase in vulnerability. It is also associated with immune dysregulation, which thereby affects vaccine responses in a sex-specific manner. Prevalence of frailty has been observed to be higher in older females compared to older males.
Previous research has indicated that frailty is not associated with either pre- or postvaccination HAI titers or antibody responses in both males and females for influenza. Moreover, the information on the impact of frailty on influenza VE was also found to be conflicting.
For COVID-19, frailty was analyzed without the consideration of biological sex. Frailty was not found to impact vaccine-induced antibody responses against the BNT162b2 vaccine. However, it was found to increase the risk for severe outcomes post-vaccination, and the VE of frail individuals was found to be lower and wane faster.
The intersection of comorbidity and sex
High occurrence of comorbidity in older adults can impact both the epidemiology of infectious diseases as well as response to vaccines. The risk of influenza-related complications as well as COVID-19-related complications was observed to be higher in older males with comorbidities compared to older females. However, the modification of the effect of multimorbidity on vaccine responses through the impact of sex is still not understood.
Conclusion
Although sex differences in influenza and COVID-19 vaccine outcomes have been identified in older individuals, a significant gap in the literature exists regarding the impact of sex-specific effects on age-related factors. Therefore, an effective roadmap is required to understand the impact of sex-responsive vaccinology in older adults. Implementation of the roadmap requires engagement among regulatory agencies, funders, academic institutions, and vaccine manufacturers. Although the current review focuses on influenza and COVID-19 vaccines, its conclusion can be implemented for other vaccines that are administered to older individuals. Further sex-responsive research is required for understanding the heterogeneity of older populations as well as providing optimal protection against diseases that vaccinations can prevent.