Sponsored Content by CN BioAug 3 2022
Overview of CN Bio
Challenges surrounding Drug Discovery
Insight into Organ-on-a-Chip Models
The PhysioMimix
Using the PhysioMimix for Non-Alcoholic Steatohepatitis (NASH)
Looking to the Future of Therapeutics
Future for CN Bio
About the Interviewee
In this interview, we speak to Dr Tomasz Kostrzewski, VP of Science and Technology at CN Bio, about their organ-on-a-chip product, PhysioMimix™, and how it can accelerate the future of drug discovery by empowering the discovery of new therapeutics.
Please could you introduce yourself and tell us about your role at CN Bio?
My name is Tomasz Kostrzewski, and I am the VP of Science and Technology at CN Bio. I am responsible for two key areas of business, one of which is the development of our new organ-on-a-chip products. This focuses on the development of new 3D in vitro perfused tissue models of human organs and the bioengineering platforms that they are cultured within. Secondly, these are offered as services, so I have a research services team that runs those contracts research programs for our clients in-house, in our labs, in Cambridge.
CN Bio is a leading bioengineering company specializing in innovative lab technologies. Why was CN Bio founded, and what are some of the company’s core aims and missions?
CN Bio were founded in 2009 as a spin-out company from the University of Oxford. Since then, we have incorporated intellectual property from a number of institutes, but most prominently from the Massachusetts Institute of Technology (MIT) in the USA. With the IP that CN Bio took on from MIT, we started building a Liver-on-a-Chip (LOAC) approximately a decade ago, and that has expanded over the years.
We have now created models of numerous human tissues and organs, including the liver, the lungs, the intestine, the immune system, and some work on the kidneys. Ultimately, our mission is to create a wide range of tools for laboratory scientists to produce translational pre-clinical data and allow them to develop new therapeutics faster for patients.
The process of developing new drugs is very, very slow. At CN Bio, we believe that standard drug development processes are broken. Frequently they fail to accurately identify whether a molecule or a therapeutic is efficacious, or whether it is toxic to humans. To put it simply - by having better, more accurate, more human-relevant pre-clinical models, we can make better decisions faster about which therapeutics to pursue and which to avoid.
Introducing the benefits of a human-relevant organ-on-a-chip approach to drug discovery - CN Bio.
The drug discovery sector has seen an increase in tension in recent years. There are still so many hurdles that need to be overcome. What do you believe to be some of the biggest challenges currently facing drug discovery?
The drug discovery industry has progressed a lot in the last few years. One trend that we have observed is the rise of a wide range of new modalities. Around a decade ago, the pipeline of most pharmaceutical companies was filled with small molecules. Now, they have everything from small molecules, large molecules, small peptides, siRNAs, ASOs, Adenoviral vectors - even gene-editing technologies. There are a whole plethora of different approaches to target different disease states, and some of these newer modalities are very, very human-specific. Where their targets are not expressed in other species, testing these therapeutics using standard in vivo pre-clinical models is not appropriate. Organ-on-a-chip (OOC) technology circumvents this workflow bottleneck, providing a way to understand target engagement, predict therapeutic efficacy, and flag off-target human-specific toxicity.
Secondly, there is a dominant need for improved models of the human immune system. Whether that is in the oncology space or in chronic diseases, the development of therapeutics that target the immune response represents an ever more popular approach. Modelling the human immune system, however, is challenging. It is made up of a phenomenally complex, intricate network of events with a wide variety of innate and adaptive responses that are very unique to humans and very different from other animal species.
The classic analogy for studies investigating the human immune system is that we are still ‘scratching at the surface.’ There are new parts of the immune system that are still being discovered and different roles identified for different cell types. When it comes to immune cells, the typical idea is to imagine them floating through the peripheral blood but, in reality, every organ has its own unique immune population. A certain immune cell might be present in your lungs but may also be in the liver where it will perform a varying set of functions. To try and recapitulate this, and then modulate it, is a significant challenge. This is particularly a problem when we consider all the different immune pathways that may be altered in a patient suffering from multiple chronic diseases. As a result, the development of models that precisely recreate immunological processes to test an ever-growing range of immunomodulatory therapeutics and enable their progression into the clinic remains a big challenge for the whole sector and an area of particular interest to us.
Finally, there is a general - and growing - trend towards patient-specific or population-specific precision medicine, which is extremely valuable. Given that everybody is unique and different people need tailored therapeutics, it is important to acknowledge that such an approach is extremely logistically and financially challenging. It is simply not possible to generate a unique therapeutic for every patient, for every human disease in the world. It is, therefore, more essential to generate therapeutics that are useful for vast populations or more importantly, combinations of therapeutics tailored for specific patient cohorts. The ability to study different treatment combinations on human-relevant cellular models is another key application for our PhysioMimix technology.

Image Credit: CN Bio
At CN Bio, you focus on developing OOC models that generate translatable pre-clinical data. Can you tell us more about what OOC models are and their role in accelerating the drug discovery process?
OOC models - which are also known as microphysiological systems - are small fluidic devices that generally hold a three-dimensional culture of human cells. Typically, we culture physiologically relevant combinations of cells that have previously come from a patient to mimic the interactions that occur within an organ or tissue. These 3D tissue structures are then perfused using microfluidics to mimic the flow of blood moving through, across or around a tissue structure to provide nutrients, remove waste and provide important biomechanical stimuli. We typically try and incorporate the immune system into our 3D tissue models so we can simulate immunological responses too.
CN Bio develops single organ models, where perfusion recirculates through the organ and multi-organ systems where two or more organs are fluidically linked together. Multi-organ systems enable us to simulate processes such as drug absorption and metabolism to predict bioavailability or to understand interactions between organs, such as on and off-target effects, or inflammation, which drives disease and causes unexpected toxicities. To date, animals, which are poor predictors of human outcomes, have been depended on to provide these insights. Now we can provide a rapid, usable, cost-effective, and more human-relevant alternative.
It is one thing building a detailed and elegant model of a human organ or tissue - but if this cannot be reproduced easily in another lab, by another operator, it has very little value. As such, we undertake a lot of work around usability and reproducibility so that we can disseminate our robust and reliable solutions around the world.
OOC models also reduce the dependence on animal testing in laboratories. What are some of the other advantages of using OOC models compared to others frequently used within life sciences research, such as traditional 2D cell cultures and animal models?
One of the key messages here is that OOC models are a key tool in the toolbox, but should never be viewed as a simple replacement for animals, or for traditional 2D cell cultures. We believe that to be successful, it is important to use all of the available tools and complement their use with bioinformatics and computational modelling approaches. Ultimately, the combination of these tools and the insights they deliver will enable researchers to make better informed decisions to withdraw or re-engineer pre-clinical drugs that are flawed early and to progress those that offer the greatest promise with more confidence.
In our opinion, OOC technology complements other technology by enabling users to study things that they cannot using other pre-clinical approaches. Animals, for example, metabolise differently to humans. Their livers express very different liver enzymes or ratios of liver enzymes compared to human liver. Our human LOAC, however, expresses all of the right CYP enzymes and the right transporters. The upshot of this is that when our LOAC produces metabolites, these are the same as the metabolites that would be produced in a human, and if toxic, we will see this too to avoid unexpected surprises in the clinic.
Traditional 2D cell culture assays are typically performed using immortalized cell lines grown in monolayers. They are relatively cheap, easy to grow, deliver fast and reproducible data, and can be used in high throughput screens. The downside of 2D cultures is that they often express the wrong cellular markers and are mostly generated from a cancer, or a cancerous source. All this means that although their use is very convenient, their physiological relevance is limited. OOC technology is more throughput limited and costly to run on a per well basis, but these assays more accurately recreate human physiology in health and disease using primary human cells, cultured in a 3D microenvironment over extended time periods (e.g. several weeks). This means that we can investigate the effects of chronic vs acute dosing, induce chronic diseases and study complex viral infections. If you consider COVID-19 or hepatitis B, for instance, we have been able to recapitulate the full viral life cycle of these kinds of complex infections, overcoming the limitations of 2D cultures for studying host/pathogen interactions. As such, OOC technology is better positioned on either side of the screening phases of drug discovery to identify/validate novel targets, confirm drug efficacy and check for toxicity.
The important thing to remember is that OOC technology is being successful when used with a defined context of use where key aspects of human biology need to be accurately mimicked. It is also essential to know the limitations of any new approach, as this allows you to clearly identify where these technologies offer the most value and how they compare to other tools that people might already use, have access to, or want to use.
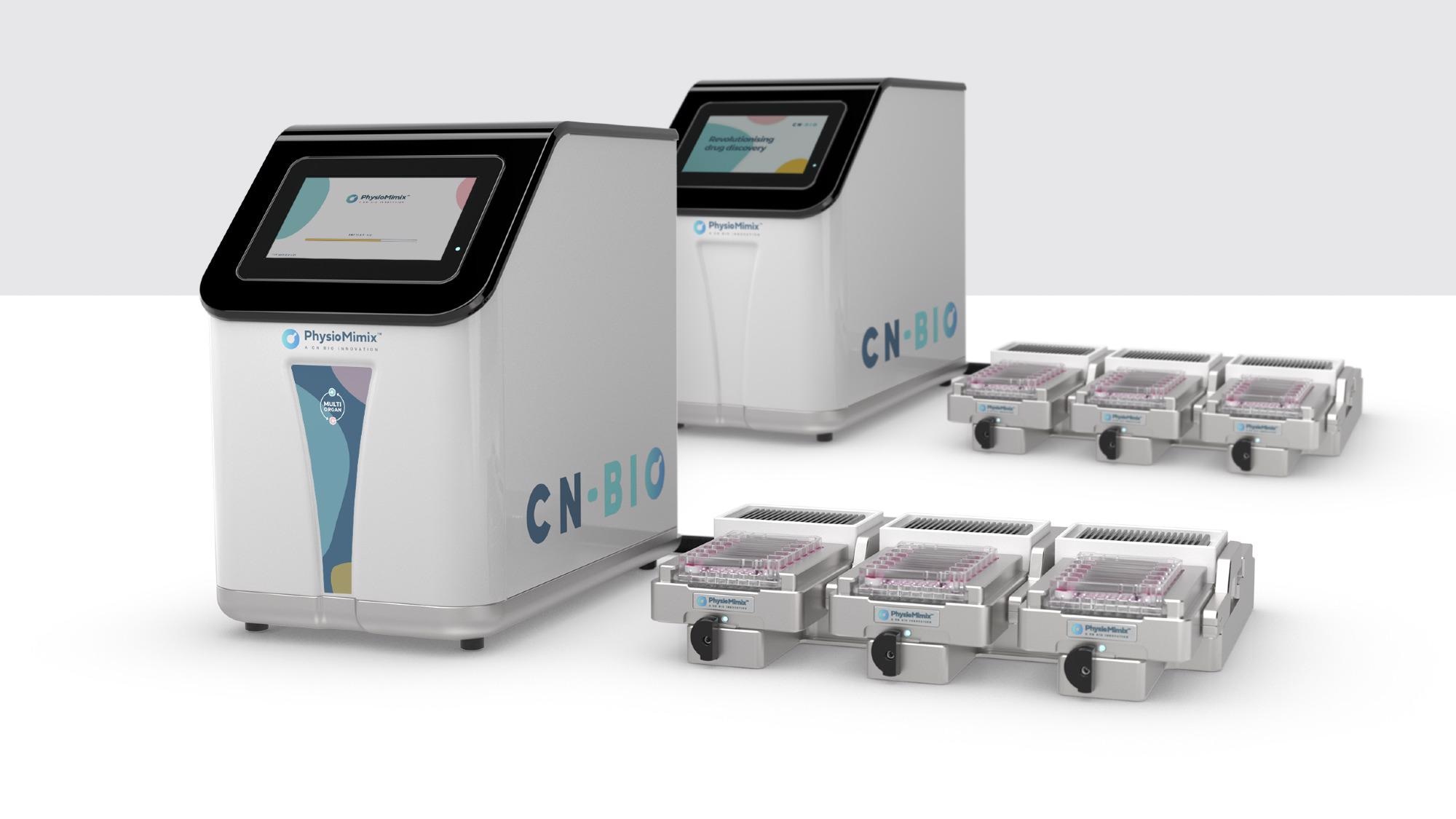
Image Credit: CN Bio
Your product, PhysioMimix, aims to create an increase in lab capabilities, which, in turn, boosts IND success. Can you tell us more about your PhysioMimix product, how it works and any advantages it has over other lab-on-a-chip technologies available?
Our PhysioMimix range is made up of a single- and multi-organ bench-top systems which have a proven track record for being robust, reliable, and usable. Our technology can be accessed in two ways: as a product to incorporate into your own laboratory workflows, or via a service from our labs in Cambridge, UK.
At CN Bio, we felt that if this technology is going to get widely adopted, it is vital to have a strong product that can be installed in any cell culture lab, and we are confident that this is what we have developed.
We have systems across the globe, all the way from Australia to the west coast of the US. The COVID pandemic meant that we needed to remotely install systems at customer sites, which proved to us that our technology is both simple to install - users can take our system out of the box and plug it in themselves - and intuitive to use - using our online training tools, customers were able to get themselves up and running OOC experiments within a couple of hours of install. Obviously, now that COVID restrictions are subsiding, on-site training is available once more.
From the perspective of support, we provide online training videos and protocols, access to our Applications Team and have recently launched a new “in-a-box” kit range to ensure that our customers can adopt an OOC approach into their workflows with ease.
PhysioMimix has a control system with a simple-to-use touchscreen interface that allows the user to set up their assays. The control system sits next to a standard cell culture incubator and the system’s docking station (for OOC plates) is housed in the incubator. Our multi-chip plates have an open-well design that look and feel like a standard cell culture plate. Our plates have an open-well design that look and feel like a standard cell culture plate. The advantage here is that this removes adoption barriers, enabling scientists to rapidly transition from 2D to 3D.
Our OOC plates contain scaffolds or inserts that support the microtissue or micro-organ growth. We offer three OOC plate types - Liver (MPS-LC12), Barrier (MPS-T12), and Multi-organ (MPS-TL6), that have been designed to meet the differing culture needs of the models that they support. These plates offer flexibility so that users can adapt our models to suit their research needs, develop their own, or even bring their own ”in house” models into a PhysioMimix format.
Your PhysioMimix systems offer single-organ, or multi-organ experiments. What are the differences between these types of experiments, and how can the ability to study multiple organs at once benefit disease modelling?
The PhysioMimix system is truly unique in the sense that users can interchange between single-organ and multi-organ experiments as they wish. A single-organ study, however, is clearly much more straightforward. Users add the cells of a particular organ or tissue type of interest into the chips to study the mechanism of disease onset, drug efficacy, the effect that the body has on a drug (e.g. drug metabolism), or drug toxicity over time.
Multi-organ assays present a number of additional challenges for which we are well placed to support. Firstly, there are clearly logistical challenges. Multiple cell types are required to form each tissue and, for some tissues, there is a pre-culture period required before being introduced into the multi-organ plate. Ensuring that multiple tissues are ready at the same time is therefore not an insignificant task.
Another important consideration for multi-organ models is the use of a common media to allow the two organs to crosstalk and communicate. We have developed a number of common mediums over the years for different organ combinations which we can share with customers.
As discussed in brief previously, multi-organ studies provide unique insights into the mechanistic interactions between two organs. For example, the on-target effects of a therapeutic can be observed in one organ as well as any off-target effects in a secondary organ. Multi-organ assays are really powerful, as they allow the user to perform in vivo-like experiments in vitro, but with the advantage that the user has complete control over all the elements. The user can control each cell type that is present, the numbers of cells, and all the time points they wish to sample at. This opens up a number of doors for people to study organ interactions in a way that they have never really been able to do before, to ask significant and deep mechanistic questions, and to help overcome inter-species issues that can mislead results and cause unexpected issues in the clinic.

Image Credit: CN Bio
You have just announced your PhysioMimix ‘in-a-box’ reagent kit for non-alcoholic steatohepatitis (NASH). With NASH being an emerging healthcare priority, how important is your technology in helping to develop new therapeutics for this disease?
Fatty liver disease, and its more advanced form, non-alcoholic steatohepatitis (NASH) is a growing problem. Approximately one-third of the Western world has some form of this disease which can lead to liver cirrhosis and liver cancer. At this point, there are no further treatment options aside from liver transplants. There have been a number of relatively high-profile failures in NASH clinical trials of molecules developed solely using traditional in-vivo models to model this disease.
Within drug discovery, NASH is usually modelled using murine models in vivo, but no one model is able to replicate all key aspects of the NASH phenotype and despite much effort, no therapeutic has made it to market.
To improve the translatability of data between the laboratory and the clinic, CN Bio has worked closely with a number of key parties over the last five years, both in pharma and academia, to develop an in vitro human model of NASH using our LOAC. A major aspect of this model is that it utilises clinical endpoints commonly observed in patients, allowing researchers to understand the effects of different therapeutic strategies.
Access to this model was only previously possible via the contract research service arm of our business, however, in response to market demand, our team has been working on a solution that enables researchers to recreate this model in their own laboratories. We have created an "in-a-box" kit which provides PhysioMimix users with all the primary cells; media; plates, and reagents they need to successfully run this assay at their own facility.
NASH-in-a-box allows us to distribute the model on a larger scale, allowing people to investigate different therapeutic strategies to target NASH and liver fibrosis, bringing their own expertise and potentially some of their own unique endpoints that they have analyzed.
Ultimately, we think that by bringing these advanced in vitro primary human models to the forefront of the research effort, new next-generation therapeutic strategies will be developed to help to tackle this growing problem.
We have seen substantial technological advancements in the drug discovery sector in recent years. Are you hopeful that we will see new therapeutics being brought to the market with continued innovation in this sector? What would that mean for global health?
It is fair to say that, amidst all the difficulties that the COVID-19 pandemic has posed, a positive light has been shone on the drug discovery and pharmaceutical industry. With the right innovation, the right need, and the right motivation, things can be done at a phenomenal speed. To put it another way, now is a key opportunity for our industry to grab that impetus, embrace novel revolutionizing technology and apply it to areas that are typically difficult to manage and target, such as chronic disease.
Oncology already has a lot of focus, but it represents an ever-growing burden with an aging population. There are other areas, such as neurological disease, which also need better pre-clinical models in order to facilitate the development of novel therapeutics.
In our opinion, it is important to embrace the toolbox of technologies now available to trial different therapeutic strategies and better predict human responses. We encourage our users to ask the right questions through their pre-clinical studies, and use a range of advanced in-vitro human-relevant approaches, combined with other more traditional approaches. By combining these approaches, researchers will be better informed so they can ultimately pick the right molecules to take forward to clinical development.
As we have seen in a lot of diseases, a combination of treatments is likely to be needed. Unfortunately, it is not going to be as simple as a single-target ‘magic bullet’, particularly in chronic diseases; as well as reducing inflammation you may need to assess the underlying metabolic problem or cause of a particular issue. Therefore, having the tools to assess those efficiently and rapidly is going to be vital.

Image Credit: Black Salmon/Shutterstock.com
What do you believe the future of organ-on-a-chip studies will look like? Do you believe more laboratories will turn to this technology to help further their discovery processes?
I believe that that is already happening. Drug attrition rates are huge and the root cause of this is the inability of traditional experiments to predict a medicine’s safety and efficacy. In the last few years, we have seen a real shift towards the adoption of OOC technology across a wide set of disciplines in the pharmaceutical industry to help address this inefficiency. CN Bio works with researchers throughout the drug discovery process; from toxicological issues to target identification and validation.
What we do expect to see in the coming years is that regulatory agencies will become more educated on the value of these technologies and, as a result, encourage more pharmaceutical companies to use these technologies in their IND submissions. From this, we will see the growing value of how these effectively make decisions about whether to progress a molecule or not.
In the longer term, there will be regulatory guidance documents about how to use these tools alongside standard in vivo and 2D in vitro approaches. We have discussed this with regulatory agencies as these technologies will become integral to many, if not most, IND packages.
What is next for CN Bio? Are there any exciting projects that you are involved in coming up?
We have a raft of projects on the go. Firstly, we will continue to work and invest in all the key OOC tissue models already built, such as our liver, intestine, lung, and oncology models. For example, some really exciting developments are coming through concerning our intestine model, including examining different sources of primary cells. All of our models typically use primary cells, and we are working ever-more-closely with the providers of those cells.
We are also interested in working with stem cell providers because those organizations can provide patient-specific cells with particular genetic mutations. Bringing different cell types into these tissue models to make them more patient-relevant is vital, and we are continuing to develop different endpoint analytics to make them more translational also.
As we go forward, we will also continue to add new organ models into our portfolio and, through our multi-organ system, we can link these different tissue models together. Ultimately, we are committed to building a body-on-a-chip style technology where you could have multiple different tissues fluidically linked and thus could be used to assess systemic toxicity or bioavailability and distribution. The user could put a compound into the system and simply watch which organ is targeted and what effects the compound has on multiple cell and tissue types.
Where can readers find more information?
Check out our website: cn-bio.com/physiomimixooc
Follow us on Twitter and LinkedIn!
About Dr. Tom Kostrzewski
Dr Kostrzewski is responsible for biological tissue model development, applications for these models and collaborative research projects with academic and commercial partners. With more than 15 years of experience in molecular and cellular biology research, Dr Kostrzewski has a PhD in Molecular Immunology from Imperial College London and experience working within large pharma developing biopharmaceutical therapeutics.
He has published more than twelve peer-reviewed scientific articles and numerous patents in the last three years, and managed multiple grant-funded collaborative projects.