Historically, MPXV has long been endemic in regions of sub-Saharan Africa; hence, researchers knew little about its ecology, epidemiology, and transmission. However, the World Health Organization (WHO) declared the 2022 MPXV outbreak a public health emergency of international concern soon after ~52,090 confirmed MPXV cases across 100 countries. Perhaps the current MPXV outbreak has been sustained due to efficient human-to-human transmission.
Considering this data, it becomes crucial to enhance MPXV surveillance, better understand its transmission routes, initiates targeted awareness campaigns, especially for at-risk populations, increase the availability of diagnostics, and intervene to mitigate the current outbreak via scientific countermeasures.
MPXV ecological habitats
Ecological niche models (ENMs) have found rope squirrels (Funisciurus spp.), but not giant pouched rats, a significant predictor of MPXV’s geographical range. Accordingly, ENM-predicted areas have more MPXV cases in humans, as confirmed by epidemiological studies. MPXV is the only known orthopox virus (OPXV) circulating in West and Central Africa, yet, the possible presence of other OPXVs hinders measurements of MPXV prevalence. Researchers have isolated MPXV from a rope squirrel and a chimpanzee, but no study has documented reverse spillover in domestic animals. The recent detection of OPXV antibodies in a domestic pig in the Democratic Republic of Congo (DRC) pointed to the zoonotic and cross-species potential of OPXVs. Overall, the range of the reservoir host complex of MPXV remains unknown.
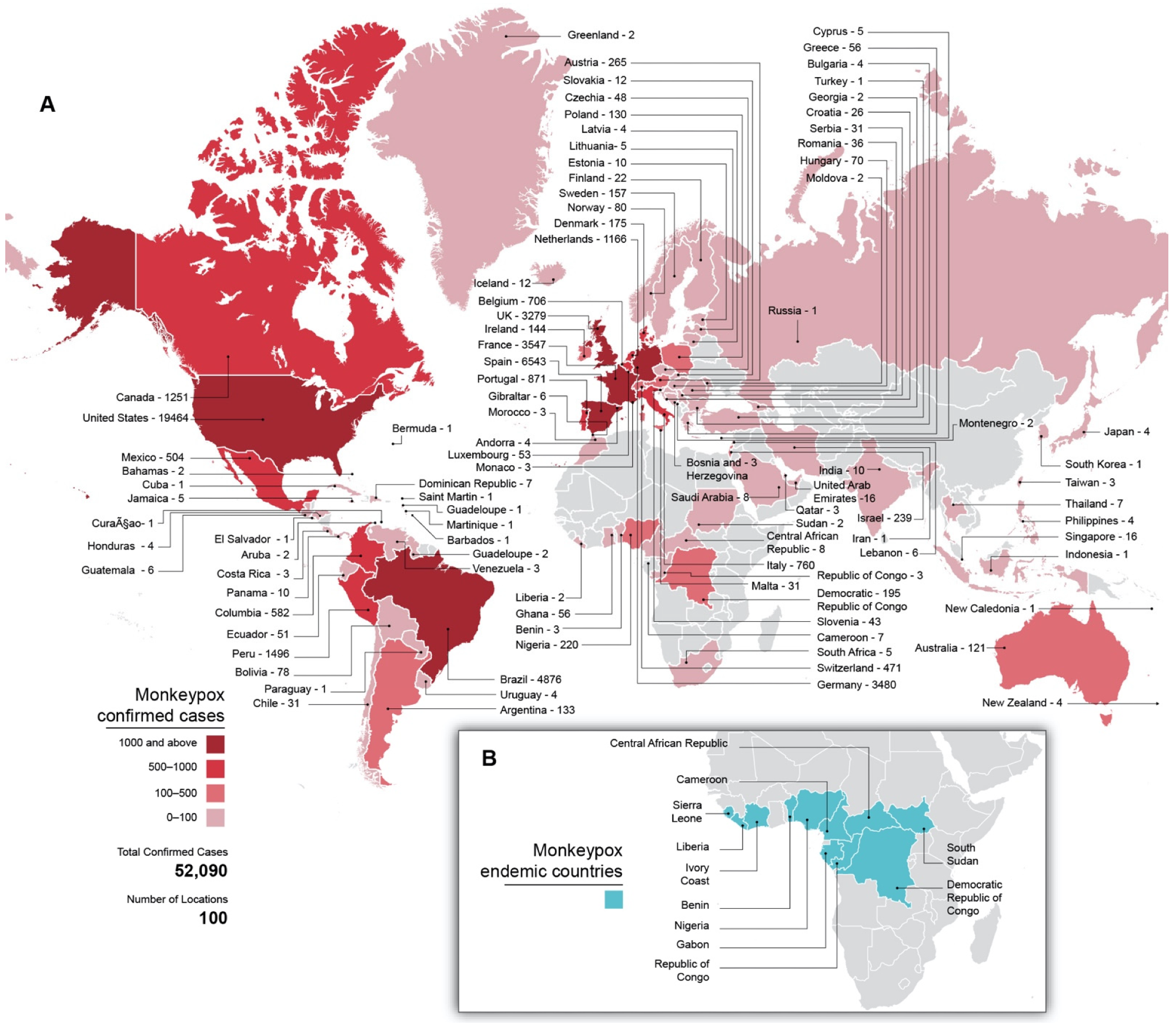 Global distribution of MPX cases. (A) MPX cases per country in the current outbreak through 1 September 2022, as well as total, confirmed cases and affected countries. Countries are colored according to case counts. Gray shading indicates no known cases. (B) Countries historically endemic for MPXV. Gray shading indicates non-endemic countries.
Global distribution of MPX cases. (A) MPX cases per country in the current outbreak through 1 September 2022, as well as total, confirmed cases and affected countries. Countries are colored according to case counts. Gray shading indicates no known cases. (B) Countries historically endemic for MPXV. Gray shading indicates non-endemic countries.
Zoonoses or MPXV spillover
Researchers have posited several potential routes of MPXV zoonotic transmission, including direct contact with dead or sick animals, animal bites and scratches, eating bushmeat, and indirect MPXV transmission from animals via respiratory droplets.
There was a 20-fold increase in MPXV transmission in the DRC between 2007 and 2007. Due to enhanced surveillance, cessation of smallpox vaccination in the 1970s, which provided cross-protection against MPXV, and waning immunity in previously vaccinated populations likely made 177.62 million Nigerian population more susceptible to MPXV infections by 2018. Subsequently, the WHO included Cameroon and Nigeria in the list of countries endemic to MPXV. Nevertheless, repeated spillover events and not the human-to-human transmission are likely sustaining several recent MPXV outbreaks.
Atypical MPXV transmission
The ongoing 2022 MPXV outbreak unfolded atypically, showing exponential growth with low case fatality ratio (CFRs) and continuous human-to-human transmission. The estimated reproduction number of MPXV was 2.43 in Italy but rose to 1.29 through July 2022. Sequencing data have confirmed that clade 2B MPXV undergoing continuous microevolution caused the recent outbreak. Notably, MPXV has spread outside the endemic areas, disproportionately affecting men-having-sex-with-men (MSM).
Unlike smallpox, which spreads primarily via respiratory droplets, MPXV transmits via respiratory droplets, contact with bodily fluids, lesions, and fomites. It also has the potential to transmit vertically. Up to 13% of MPXV cases were transmitted via unusual routes in the 2022 outbreak, thus, presenting atypically. Since these cases were more difficult to diagnose, they resulted in more significant outbreaks.
Even hospital-associated MPXV outbreaks are severe and long-lasting. Therefore, it is essential to maintain hygienic hospital practices and use appropriate personal protective equipment (PPE) and patient isolation to minimize within-hospital MPXV transmission.
Historical research on MPXV was focused on clade 1 in the DRC though there have been longitudinal surges in the documentation of clade 2 MPXV infections. Infections with clade 2B MPXV in the current outbreak had prolonged periods between symptom onset and diagnosis, resulting in increased transmission.
Conclusions
Since historical times, sub -Saharan African countries have borne the burden of MPXV, but high background levels of OPXV antibodies in MPXV-endemic areas suggest that many MPX cases go undetected. In addition, the absence of point-of-care diagnostics prevents the affected people from reporting the disease through the integrated disease surveillance and response system. In order to address the public health burden of MPXV, concerted efforts are required. Most importantly, there is a need to deploy different strategies in endemic and non-endemic areas.
In endemic areas, children are most affected. Hence, healthcare providers should be aware of the distinguishing features of MPXV (from chickenpox) to facilitate timely and accurate diagnoses, allowing for quicker isolation of the infected children. In addition, there should be concerted efforts to vaccinate healthcare workers and populations at risk (e.g., children in forested areas) to prevent the incidence and further spillover and mitigate the size of MPXV outbreaks. A long undetected MPXV circulation will likely result in more efficient replication and human-to-human transmission.
Human immunodeficiency virus (HIV) research data suggests that increased stigma towards HIV-afflicted people resulted in lower levels of medication adherence and usage of health services. Although MPXV is not a disease of MSM and being an MSM is not a risk factor; yet, MPXV is spreading efficiently through MSM networks. Therefore, there is an urgent need to work with established leaders in MSM communities in endemic countries and develop feasible and sensitive interventions to mitigate the current MPXV outbreak and future MPXV cases in these areas.