The health burden of SARS-CoV-2 infections among Western nations reduced in 2022, attributed to COVID-19 vaccinations and Omicron VOC predominance. However, a sizeable proportion of individuals continue to be unvaccinated, among whom COVID-19 severity during the Omicron wave is not thoroughly characterized.
 Study: Disease severity of unvaccinated SARS-CoV-2 positive adults less than 65 years old without comorbidity, in the Omicron period and pre-Omicron periods. Image Credit: Ground Picture / Shutterstock
Study: Disease severity of unvaccinated SARS-CoV-2 positive adults less than 65 years old without comorbidity, in the Omicron period and pre-Omicron periods. Image Credit: Ground Picture / Shutterstock

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
About the study
The present register-based study evaluated COVID-19 severity among unvaccinated adults during Omicron and pre-Omicron COVID-19 waves.
The study comprised unvaccinated Swedish residents without comorbidities, aged between 18 and 64 years, infected with SARS-CoV-2 between week 45 of 2020 and week 5 of 2022. VOC periods were those with particular VOCs detected in ≥92.0% of COVID-19 cases sequenced by whole-genome sequencing at a national level. The study outcomes were hospitalizations, severe COVID-19 or mortality associated with SARS-CoV-2 infections.
Severe COVID-19 cases were those requiring high-flow nasal oxygen or ICU (intensive care unit) admissions. Hospitalizations five days prior up to two weeks after the initial SARS-CoV-2-positive report and deaths within 2 months of SARS-CoV-2-positive reports were considered. The team obtained data on demographic and socioeconomic variables (including nationality, level of education, income, and income sources), comorbidities, medications prescribed in the previous five years, care requirements, hospital admissions, discharge codes, deaths, and causes of death.
The public health agency of Sweden provided data on COVID-19 vaccination status. Nationwide registry data were compiled by the National Board of health and welfare of Sweden. Data on ICU admissions were obtained from the Intensive Care Registry of Sweden, and socioeconomic data were obtained from the Swedish longitudinal health insurance and labor market studies database. Logistic regression modeling was performed, and the adjusted odds ratios (ORs) were calculated.
Results
Using whole-genome sequencing, the Alpha VOC period was identified as that between week 14 and week 21 of 2021. The mixed Alpha VOC-Delta VOC period was identified between week 22 and week 27 of 2021. The Delta VOC period was identified between week 28 and week 49 of 2021. The mixed Delta VOC-Omicron VOC period was identified between week 50 of 2021 and week 1 of 2022, and the Omicron VOC period was between weeks 2.0 and week 5 of the year 2022.
Additionally, a pre-SARS-CoV-2 VOC period between weeks 45 and week 51 of the year 2020 and the mixed pre-VOC and Alpha VOC period between week 52 of the year 2020 and week 13 of the following year were included. Out of 788,895 adult COVID-19 patients, hospitalizations and deaths increased gradually from the pre-VOC COVID-19 wave to the Alpha VOC wave and Delta VOC wave, reducing thereafter during the SARS-CoV-2 Omicron VOC wave. Among 15,179 hospitalized COVID-19 patients, the percentage of severe COVID-19 cases and deaths increased up to the Delta wave, returning to pre-variant wave levels during the SARS-CoV-2 Omicron VOC wave.
The percentages of unvaccinated individuals diagnosed with COVID-19 for the first time were 100% and <20% during the pre-variant and Omicron periods, respectively. The percentages of females infected during the pre-variant COVID-19 wave, Alpha wave, Delta wave, and Omicron wave were 53.0%, 48.0%, 49.0%, and 51.0% with median values for age (in years) of 40, 38, 32, and 35, respectively. COVID-19-associated hospitalizations during the pre-variant wave, Delta wave, and Omicron wave were 1.6%, 3.9%, and 0.3%, respectively, with most hospital admissions among individuals aged between 50 and 64 years, respectively, across all waves.
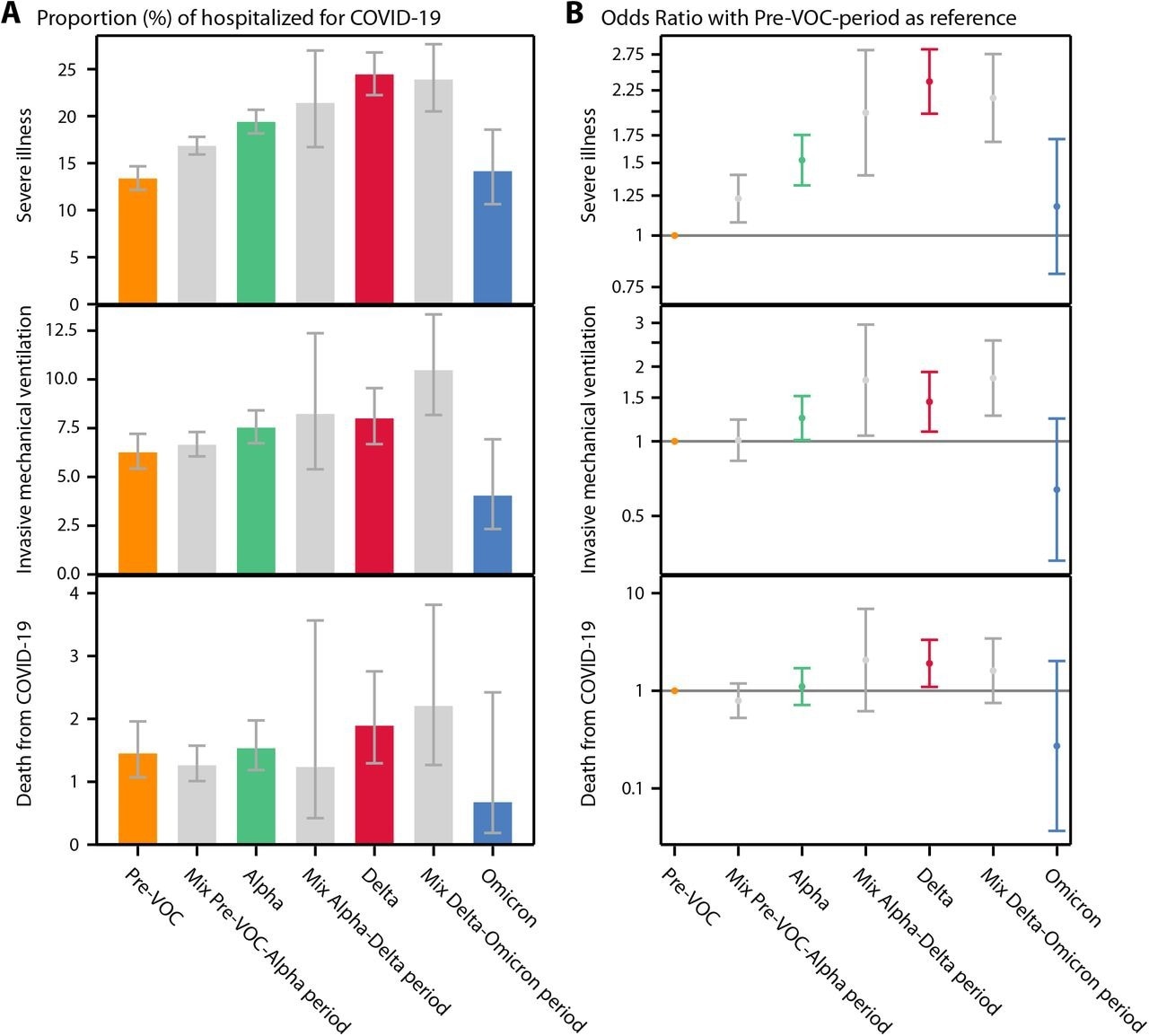
Proportions of study outcomes among patients hospitalized for COVID-19 with 95% confidence intervals according to VOC predominance. B) Odds ratios for study outcomes among patients hospitalized for COVID-19 with 95% confidence intervals adjusted for age, sex, and socio-economic status with the Pre-VOC period as reference.
Compared to the pre-variant wave, the aOR values for hospital admissions during the Alpha wave, Delta wave, and Omicron wave were 1.7, 3.1, and 0.3, respectively. Likewise, mortality rates during the pre-variant wave, Delta wave, and Omicron wave were 0.03%, 0.1%, and 0.01%, respectively, with most deaths among individuals aged between 50 and 64 years across all waves. The aOR values for COVID-19-associated deaths during the Alpha wave, Delta wave, and Omicron wave were 1.8, 4.4, and 0.3, respectively.
Severe COVID-19 cases during the pre-variant wave, Delta wave, and Omicron wave were 13%, 23%, and 14%, respectively. The median value for the age of severe Omicron infection patients was 53.0 years, and 38.0% were women. COVID-19 severity was more significant among individuals aged between 35 years and 49 years and between 50.0 years and 64.0 years compared to adults aged below 34 years. The aOR values for COVID-19 severity during the Alpha wave, Delta wave, and Omicron wave were 1.5, 2.4, and 1.2, respectively. Using the Delta wave for reference, the aOR values for severe COVID-19 cases, invasive-type mechanical ventilator requirements, and deaths during the Omicron wave were 0.5, 0.5, and 0.10, respectively.
Overall, the study findings showed lower hospitalizations and deaths among unvaccinated adults aged below 65 years during the Omicron wave, compared to prior VOC waves; however, the proportion of severe COVID-19 cases was similar during the Omicron and pre-Omicron periods. The findings underpin ongoing efforts to prevent COVID-19-associated hospitalizations.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.