The study's results indicate that the community composition and abundance of gut microbiota differed significantly between individuals with diabetic neuropathy and patients with diabetes who remained neuropathy free for ten years or more.
They used these results to train an algorithm to distinguish between the two pathological states, improving diagnostic accuracy.
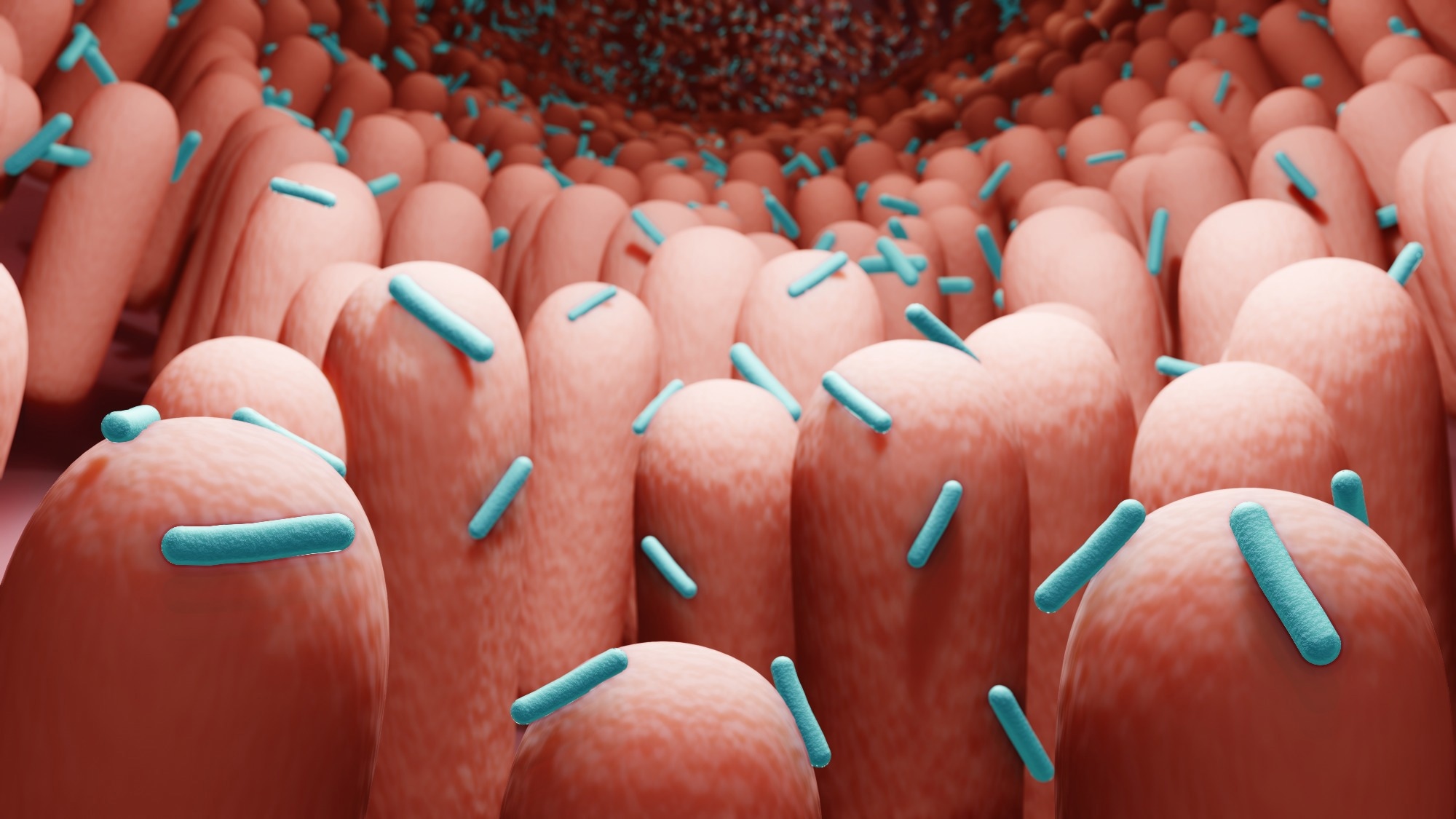 Study: Alterations of gut microbiota in biopsy-proven diabetic nephropathy and a long history of diabetes without kidney damage. Image Credit: ART-ur/Shutterstock.com
Study: Alterations of gut microbiota in biopsy-proven diabetic nephropathy and a long history of diabetes without kidney damage. Image Credit: ART-ur/Shutterstock.com
Diabetic neuropathy and gut microbiota
Diabetes is a condition characterized by abnormally high blood glucose. Diabetes is ubiquitous, with reports from China indicating 11.2% between 2015-2017 and more recent global announcements estimating that more than 10% of individuals between the ages of 20-79 are afflicted.
Diabetic neuropathy (DN) is nerve damage that occurs alongside diabetes, with symptoms ranging from mild discomfort to death.
Research has estimated that almost half of all people with diabetes suffer from DN, making it the foremost cause of end-stage renal disease (ESRD) globally. Studies, including those on kidney diseases, have elucidated the participation of gut microbiota in the initiation and progression of numerous diseases.
Gut microbiota comprises between 500-1,000 species of bacteria living symbiotically in the gastrointestinal tracts responsible for several essential vitamins, metabolites, and immune function.
Some proteins, metabolites, and toxins have been suggested to play a role in kidney health. Still, research has ignored the association between patterns and functional changes in gut flora and diabetes pathology.
About the study
In the present study, researchers aimed to characterize the gut microbiota of patients with DN compared to those with type 2 diabetes but without neuropathy (T2DM). They further developed a model capable of using fecal sample analyses to distinguish between the two groups.
Researchers began by defining three cohorts – 35 DN patients whose status was confirmed postmortem via renal biopsy, 40 T2DM patients who remained DN-free for ten years or more, and 40 age- and sex-matched healthy adults (NC). Fresh fecal samples were collected and stored for subsequent DNA analyses.
DNA was extracted, purified, and amplified using Next-Generation Illumina sequencing to build a microbial DNA library for each cohort. Researchers measured α diversity per sample and β diversity across cohorts. They then used linear discriminant analysis effect size (LEfSe) analysis to identify biomarkers significantly different between the three groups.
Pathological classification of DN was carried out by evaluating kidney damage by mesangial matrix (M), glomerular volume (G), glomerulosclerosis (S), glomerular basement membrane (GBM), and interstitial lesions (I).
A scale of one to three was used to indicate the severity of renal damage. Finally, researchers trained and tested a Random Forest machine-learning model to classify and predict the prevalence of DN or T2DM using gut microbe community composition.
Study findings
Researchers identified 844 operational taxonomic units (OTUs) in the present study. The NC cohort had the highest species diversity, with 616 OTUs compared to 480 for T2DM and 450 for DN.
The DM and DN cohorts had 113 and 102 unique OTUs not present in any other group. Richness and diversity indices revealed that while the species richness of all three cohorts differed significantly from the others, no significance was observed in cohort-specific diversity measures. However, the α diversity of patients with diabetes was found to be consistently higher than in healthy adults.
These results suggest that gut microbial communities of T2DM and DN patients were significantly altered from NC individuals.
Taxonomic classification using the LEfSe algorithm revealed that healthy adults had much higher densities of five families, three orders, and two classes when compared to diabetes patients.
"The numbers of Christensenella, Clostridium-XIVa, Eisenbergiella, Flavonifractor, and Clostridium-XVIII in the DN group were significantly increased (all P < 0.05), while the numbers of butyric-producing bacteria, Bacillus, Enterobacter, Trichospira, and Rosacella were significantly decreased in the DM group and DN group (P < 0.05)."
Results indicate that the abundance of only one genus (Clostridium-XVIII) was sufficient to accurately classify an individual as positive for DN – healthy adults had significantly higher abundances than DN patients.
Gemmiger spp. was similarly sufficient in distinguishing NC from T2DM cohorts, while DM and T2DM cohorts could be separated by evaluating the richness of Flavonifractor and Eisenbergiella genera.
The Random Forest Model trained using the above data predicted DN patients from age and sex-matched healthy individuals with an 84.2% accuracy. Similarly, the model could identify between DN and T2DM individuals with 88.6% and 90.9% accuracy.
"Because diabetic nephropathy is mostly clinically diagnosed, many patients with diabetes complicated with chronic kidney disease are easily misdiagnosed as diabetic nephropathy, resulting in phenotypic heterogeneity."
This model thus shows clinical promise in the accurate and timely diagnosis of DN and early therapeutic intervention.
Conclusions
In the present study, researchers used gut microbe analyses to identify functional changes and imbalance patterns in individuals with diabetic neuropathy. Their research revealed that gut microbial communities in patients with diabetes were starkly different from healthy adults.
The presence and abundance of specific bacterial genera were sufficient to elucidate a fecal sample's condition (healthy, T2DM, or DN).
They used their results to build a machine-learning model that can analyze fecal samples and accurately diagnose both diabetes, and provides an early warning for diabetic neuropathy.
This helps overcome the limitations of current diagnostic tools, which regularly misidentify chronic kidney disease as DN.
While this was a cross-sectional study with small sample size, a more extensive follow-up study might set the stage for faster and more accurate type 2 diabetes diagnosis in the future.