Sponsored Content by BGI GenomicsReviewed by Olivia FrostApr 12 2023
To kick off the first-ever global colorectal cancer (CRC) awareness report, it is important to note that there were over 1.9 million new cases of colorectal cancer in 2020, making it the third most common cancer worldwide.
The lack of symptoms associated with CRC means that diagnosis often occurs at an advanced stage, which is why it is so often referred to as a “silent killer.”
When CRC is detected at an early stage, the five-year relative survival rate is approximately 90%. However, only 4 out of 10 CRC cases tend to be identified at this early stage.
Although genetic factors may mean that certain individuals may be predisposed to CRC, a significant number of cases are closely associated with increasing income and its corresponding risk factors, such as physical inactivity, obesity, alcohol, and smoking.
BGI Genomics: A Roundtable Discussion on Colorectal Cancer Detection
Consequently, the burden of CRC is now moving into low-income and middle-income nations as their income rises. These countries require regular CRC screening to improve survival rates and control expenses, considering that cancer takes 10-15 years to develop.
Recognizing these concerns, BGI Genomics has launched a global colorectal cancer awareness report to help understand the current state of CRC awareness, as well as attitudes and actions concerning CRC screening for both average-risk and hereditary genetic-risk groups on a global scale.
The research encompasses 1817 participants from the United Kingdom (Western Europe), Hungary (Eastern Europe), Saudi Arabia (Middle East and Africa), Thailand (Southeast Asia), the Chinese mainland, and Hong Kong (North Asia).
Of the above, Hungary had the highest global rate of colorectal cancer in 2020, based on data from the World Cancer Research Fund.
The following are the key findings of the report:
- 21.5% more respondents name breast cancer as a top three cancer versus those who mention CRC. The U.K has the largest CRC awareness gap with 72.0%.
- 51.5% of respondents feel that there is insufficient information about CRC. In particular, the U.K. (68.3%), Hungary (65.7%), and Thailand (62.1%) feel that there is not enough information.
- 54.1% of respondents have never had a CRC test. Hungarian respondents (68.3%) are most likely to have not taken tests. These respondents also indicated that they have insufficient information about CRC.
- 69.2% of respondents are aware of colonoscopy as a screening test, while fecal tests are known by 49.5%. Fear of colonoscopy (48.2%) is the top reason holding people back from CRC screening.
- 34.5% of respondents cited cost as a barrier to CRC screening. Thailand (48.2%) and Hong Kong (46.2%) have the highest percentage of respondents concerned about costs.
- 49.5% of respondents have heard about fecal testing. The lowest percentage of respondents who had heard of fecal testing (40.6%) were aged between 35-40 years old.
- 52.5% of respondents feel that fecal testing is the easiest CRC screening test to administer, followed by colonoscopy (32.4%). The U.K. (74.6%) and Hungary (74.3%) have the highest percentage of respondents who prefer fecal testing.
- 88.8% of respondents are more willing to undergo screening after learning that early detection of CRC can result in a survival rate as high as 90%.
- 62.5% of respondents will follow their doctor’s advice to undergo CRC screening. The next most common factor is an awareness that they fall within the average risk CRC age group (47.6%).
- 55.7% of respondents are aware that a family history of CRC increases their risk. The U.K. (68.3%) is the most informed about the risks associated with CRC family history, while Thailand (46.5%) is the least informed.
- 67.2% who had CRC or a family history of CRC have taken their family members for screening. Conversely, only 31.2% of all respondents have taken their family members for CRC screening.
- 35.2% of female respondents have taken their family members for screening, compared to 27.3% of male respondents.
This report is split into three segments:
- Awareness
- Attitudes and actions towards screening for average risk groups
- Attitudes and actions towards screening for hereditary genetic risk groups
BGI Genomics has provided detailed data and information based on the findings outlined below.
Awareness
What is the impact of a CRC awareness gap?
When analyzing new cancer cases in 2020 compared to the top three cancers identified by respondents, it became clear that there was a noticeable knowledge gap regarding colorectal cancer.
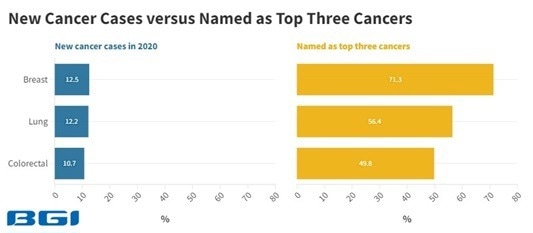
Source: World Cancer Research Fund & BGI Genomics 2023 Global State of Colorectal Cancer Awareness Report. Image Credit: BGI Genomics
Even though the gap in new breast and colorectal cancer cases is less than 2%, there is a 21.5% gap between those who named breast cancer as a top three cancer versus those who mentioned CRC. The United Kingdom has the largest awareness gap at 72.0%.
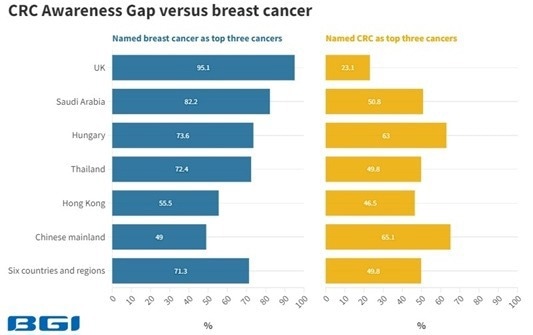
Image Credit: BGI Genomics
Moreover, 51.5% feel they have insufficient information about CRC, including symptoms and recommended screening age. In particular, respondents from the United Kingdom (68.3%), Hungary (65.7%), and Thailand (62.1%) expressed a lack of information about CRC.
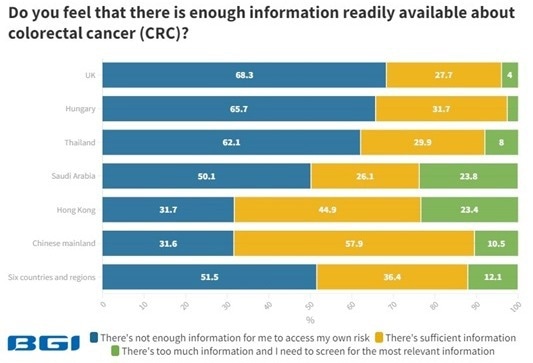
Image Credit: BGI Genomics
54.1% have never undergone CRC testing, with Hungarian respondents (68.3%) being the most likely to have never taken such tests. Interestingly, a significant number of respondents from Hungary also state that they have insufficient information about CRC.
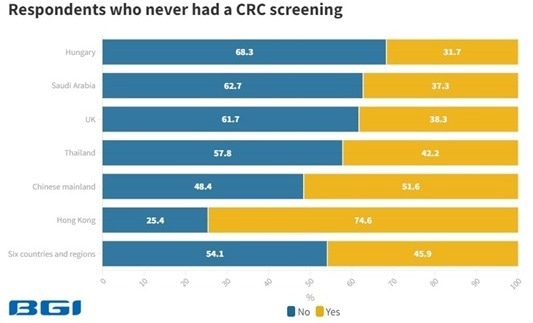
Image Credit: BGI Genomics
This lack of knowledge about CRC may contribute to the respondent’s decision not to undergo CRC screening. This is particularly concerning as precancerous polyps can be detected through regular screening to increase survival rates and reduce costs. These polyps are the abnormal growth of tissues in the colon or rectum, which can take 10-15 years to develop into cancer.
Image Credit: Louisiana Department of Health Twitter Account
Attitudes and actions towards screening for average risk groups
What is holding them back from screening tests?
The majority of global colorectal cancer screening guidelines recommend that individuals with no symptoms, family history of colorectal cancer, and average risk begin regular screening at the age of 50. However, the U.S. Preventive Services Task Force (USPSTF) guidelines issued in 2021 propose regular screening at age 45.
The main reason holding people back from CRC screening is a fear of colonoscopy (48.2%) and a fear of the results (41.4%). In particular, the Chinese mainland exhibits the highest fear rates of colonoscopy (56.9%) and results (51.6%).
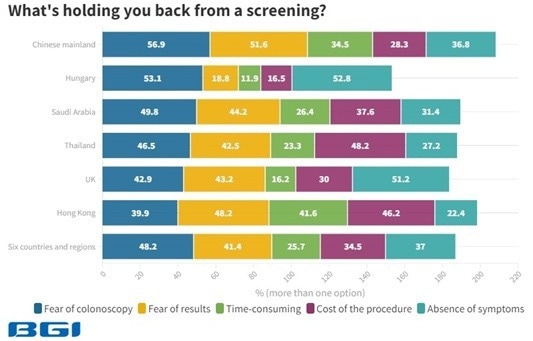
Image Credit: BGI Genomics
Additionally, 34.5% of respondents have expressed cost as a barrier to undergoing CRC screening, with the highest levels of concern in Thailand (48.2%) and Hong Kong (46.2%).
Are there alternatives to coloscopy?
Fecal testing presents itself as a cheaper, more flexible, and non-invasive alternative to colonoscopy. Unlike colonoscopy, fecal testing requires no dietary restrictions or medication changes before taking the test.

Image Credit: Mayo Clinic Twitter Account
Colonoscopy (68.2%) is the most well-known screening test relative to fecal tests (49.5%). 40.6% of respondents aged between 35-40 had heard about fecal testing, the lowest among all age groups. This indicates more work needs to be done among this age group regarding fecal testing awareness.
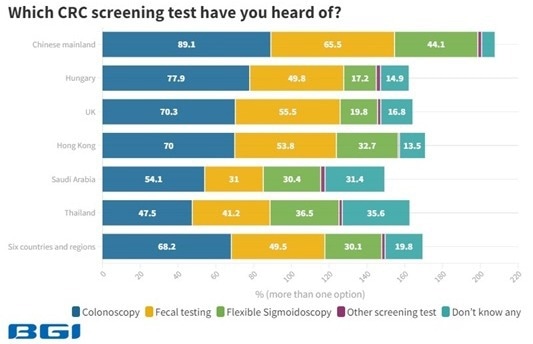
Image Credit: BGI Genomics
52.5% view fecal testing as the easiest CRC screening test to administer, followed by colonoscopy (32.4%).
The United Kingdom (74.6%) and Hungary (74.3%) have the highest percentage of respondents who prefer fecal testing. This suggests that in countries where fecal testing is more widely recognized as an advantageous screening option, there is a higher likelihood of increased uptake, particularly when the tests are more affordable.
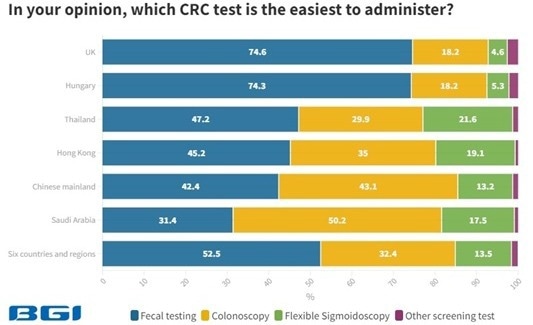
Image Credit: BGI Genomics
What is likely to encourage people to undergo CRC screening?
The most compelling reason to undergo CRC screening is the higher survival rates associated with early detection. 88.8% indicate that they are more willing to go for screening after learning that early detection of CRC leads to a 5-year relative survival rate of 90%.
However, only 4 out of 10 CRC cases are detected at this early stage.
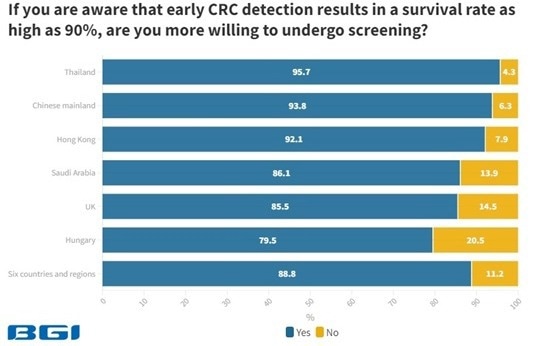
Image Credit: BGI Genomics
Advice from doctors and self-awareness are also significant factors motivating respondents to undergo CRC screening. 62.5% report that they will follow their doctor’s recommendation to undergo CRC screening.
The next most common reason is an awareness that respondents fall within the average risk CRC age group (47.6%).
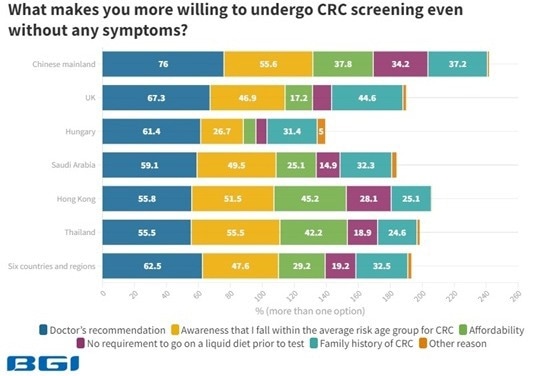
Image Credit: BGI Genomics
Attitudes and actions towards screening for hereditary risk groups
Are they making informed choices to manage their risks?
Individuals with a first-degree relative diagnosed with colorectal cancer (CRC) are at an increased risk of developing this cancer.
The National Comprehensive Cancer Network (NCCN) guidelines recommend that these family members start screening at age 40 or 10 years before the earliest diagnosis of CRC in the family.
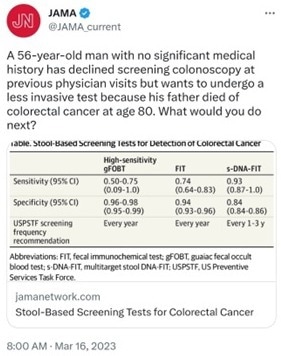
Image Credit: JAMA Network Twitter Account
55.7% of the respondents are aware that a family history of CRC increases their risk. The U.K. (68.3%) is the most informed about the risks associated with CRC family history, while Thailand (46.5%) is the least informed.
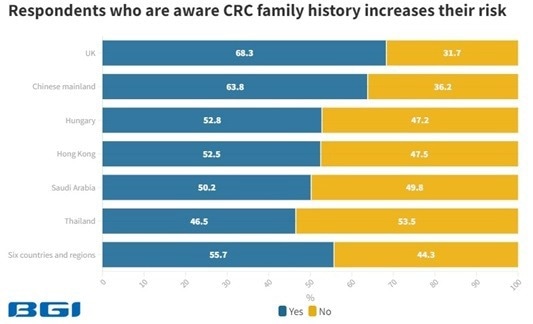
Image Credit: BGI Genomics
To help manage their risk, 67.2% of respondents who had CRC or a family history of CRC have taken their family members for screening.
Conversely, only 31.2% of all respondents have never taken their family members for CRC screening. This indicates that hereditary risk groups are more proactively managing their risk through CRC screening.
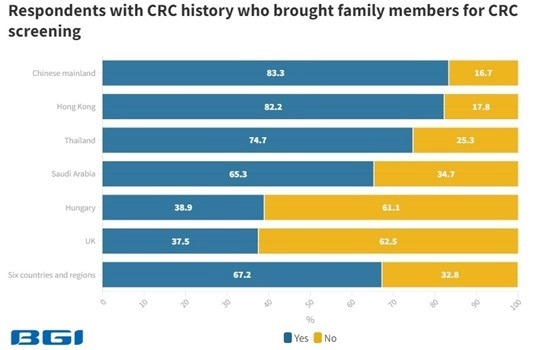
Image Credit: BGI Genomics
Female respondents are more likely to take their family members for CRC screening than male respondents, with 35.2% of female respondents having done so compared to 27.3% of male respondents.
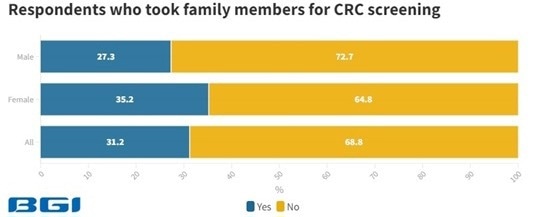
Image Credit: BGI Genomics
Concluding remarks
This report indicates that a three-pronged approach is needed to help catch up to the “silent killer” that is global CRC:
- Enhancing general awareness: 51.5% of people feel that there is insufficient information about CRC. To address this, awareness campaigns should include information on CRC symptoms, recommended screening age, and a variety of screening options such as colonoscopy and fecal tests. The 5-year survival rate of 90% for early CRC detection is also worth noting, as 88.8% of individuals are more likely to go for screening after hearing this.
- Enhancing affordability: 34.5% of people have mentioned cost as a significant barrier to CRC screening. Though colonoscopy (68.2%) is the most well-known screening test, it is cumbersome and more expensive than fecal testing, which is lesser known at 49.5%. We must first enhance fecal testing awareness to promote this more affordable option.
- Enhancing doctor’s awareness: Upon hearing their doctor’s advice, 62.5% of individuals are likely to undergo CRC screening. Therefore, doctors must be made more aware of CRC symptoms, ask the right questions to identify potential hereditary genetic risks, and offer patients a range of screening options to fit varying budgets and lifestyles. For BGI (and The Mayo Clinic), the best colorectal cancer screening test is the one that a patient is willing to undergo.
Early CRC detection offers the best outcome for individuals and healthcare policy. The treatment cost of late-stage CRC is sometimes more than ten times higher relative to early-stage CRC but with far lower survival rates. That’s why more countries or regions are promoting early screening programs. For example, the European Commission is ramping up CRC screening programs.
Yantao Li, Ph.D., BGI Genomics Director of Colorectal Cancer Screening Programme, South-East Asia.

Image Credit: EU Health Twitter Account
To select country or region-level data comparisons, please see link to access the original BGI Genomics State of Colorectal Cancer Awareness Report 2023.
BGI Genomics and COLOTECT®
BGI Genomics, headquartered in Shenzhen, China, is a top integrated global precision medicine solutions provider. BGI Genomics (300676.SZ), a subsidiary of the BGI Group, was officially listed on the Shenzhen Stock Exchange in July 2017.
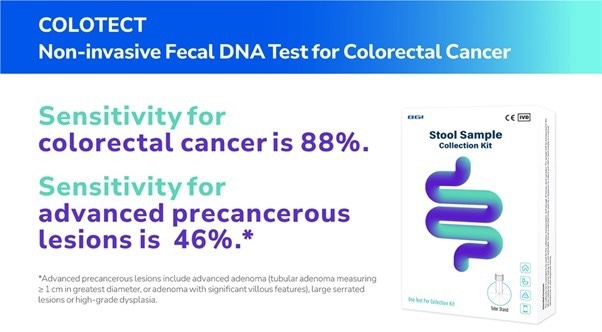
Image Credit: BGI Genomics
One of its innovative products is COLOTECT®, a non-invasive fecal DNA test designed to detect colorectal cancer (CRC) and precancerous lesions. The test employs multiplex methylation-specific PCR (MSP) technology to identify abnormal DNA-methylation biomarkers in CRC from stool samples.
COLOTECT® boasts a high CRC sensitivity of 88%, and for early detection, its sensitivity for advanced adenoma is 46%, which is superior to conventional fecal tests.
Methodology
This study was based on an online survey of 1817 respondents from Hungary (303), the UK (303), Saudi Arabia (303), the Chinese mainland (304), Thailand (301), and Hong Kong (301).
The respondents were based in their respective countries or regions and completed the survey in their local language. The survey included individuals aged between 35 to 75 years old with an equal male-to-female sex ratio.
About BGI Genomics
BGI Genomics is the world's leading integrated solutions provider of precision medicine, now serving customers in more than 100 countries.
They provide academic institutions, pharmaceutical companies, healthcare providers, and other organizations with integrated genomic sequencing, proteomic services, clinical testing, and solutions across a broad range of applications.
They have more than 20 years of genomics experience helping customers and partners achieve their goals by delivering rapid, high-quality results using a broad array of cost-effective, cutting-edge technologies, including their own innovative DNBSEQ™ sequencing technology.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.