Both sexually transmitted infections (STIs), syphilis and gonorrhoea, are on the rise in modern England, staging a comeback from the Victorian era. Over the past one year, there has been a 20 percent rise in the incidence of STIs. The rates of syphilis for example is on a 70 year high last year according to the Public Health England statistics.
The PHE England published the figures and urged the local as well as national services to up their game in prevention and treatment of STIs. The report states that there were a total of 7,137 new cases of syphilis in 2017 and this is a 20 percent rise from the year before. This number is the largest since 1949 the report says. Highest incidence is seen among adults aged between 25 and 34 years and they were one third of all the cases. The next highest incidence was seen among those aged between 35 and 44 years.
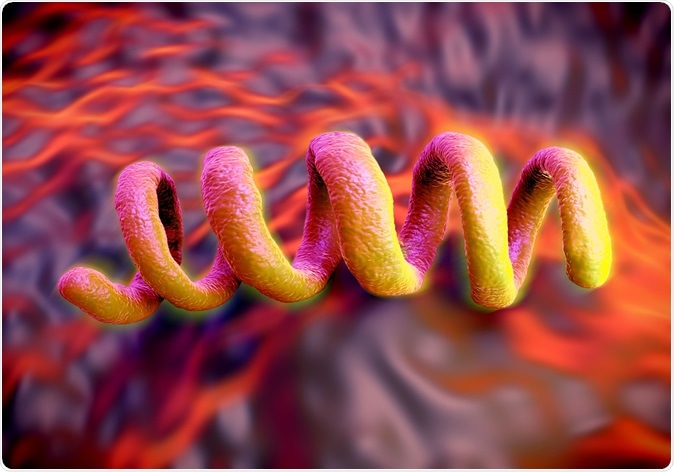
Treponema pallidum Syphilis bacterium, the bacterium responsible for the dangerous sexually transmitted infection syphilis. Image Credit: Royaltystockphoto.com / Shutterstock
The report adds that 78 percent cases were seen in men who had had unprotected sex with men. Gonorrhea too is on the rise with a 22 percent increase in the number of cases in 2017. PHE England calls this rise as “concerning”. This is mainly because gonorrhoea strains that are affecting people are becoming increasingly resistant to the antibiotics that are at hand. In March 2018 for example a man was admitted with gonorrhoea that was highly resistant to the two types of antibiotics that this bacteria is most sensitive to. The man had travelled to south-east Asia from where he could have got the infection. Since then the PHE has directed GPs to refer the suspected cases of gonorrhoea they encounter to specialist sexual health services (SHS).
There has been a rise of 3 percent in SHS attendance between 2016 and 2017 (3.2 million in 2016 and 3.3 million in 2017). The numbers have risen by 13 percent in the last five years says the report. Councillor Izzi Seccombe, chairwoman of the Local Government Association’s Community Wellbeing Board said in a statement that this major rise in attendances to the SHS has put a strain on the resources. She said, “There is no time for complacency… Unless greater recognition and funding is given to councils to invest in prevention services, a reversal in the encouraging and continuing fall in STIs is now a real risk. Health inequalities will remain and councils may be unable to respond effectively to unforeseen outbreaks.” She called on the government to reverse the cuts to the councils so that they can meet the rising requirements.
On the other, there has been a reduction in number of cases of chlamydia infection by 8 percent. According to the PHE, most of this decline has been seen in the SHS where testing for chlamydia has come down by 61 percent since 2015. They speculate that this reduction is not due to reduction in incidence of the infection but lack of testing. The recommendations state that all young women should be tested for chlamydia when they access contraception. The recommendations also emphasize on high-quality relationships and sex education at schools.
According to Dr Gwenda Hughes, consultant scientist and head of the STI section at PHE, the long term health consequences of STIs are many. She explains that there is a high risk of infertility, pelvic inflammatory disease and danger to the unborn babies. The risk is to self as well as to present and future sexual partners she explained. She said that there should be consistent and correct use of condoms with new and casual sexual partners as well as regular check-ups and testing to determine and treat these infections early.