The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the infectious agent that causes coronavirus disease 2019 (COVID-19), broke out in December 2019 and is still spreading rapidly. The World Health Organization (WHO) and other major national and international public health bodies have branded the virus's spread as a worldwide pandemic, with over 57.1 million people infected and over 1.36 million deceased.
As this global health crisis evolves, scientists have been racing to provide insight into the virus structure to find a therapeutic target that can mitigate its impact on those with severe cases.
Dr. Kara Fitzgerald, a researcher at the Institute for Functional Medicine in the United States, has explained the role of furin protease in developing severe COVID-19 illness. Conditions tied to elevated furin levels – including obesity, hypertension, and diabetes – show overlap with vulnerability to more severe forms of COVID-19. Dr. Fitzgerald's study, which appeared in The Permanente medical journal, was published in September 2020.
What is furin protease?
Proteases describe a large group of diverse hydrolytic enzymes. They catalyze proteolysis, the breakdown of proteins into smaller polypeptides or single amino acids.
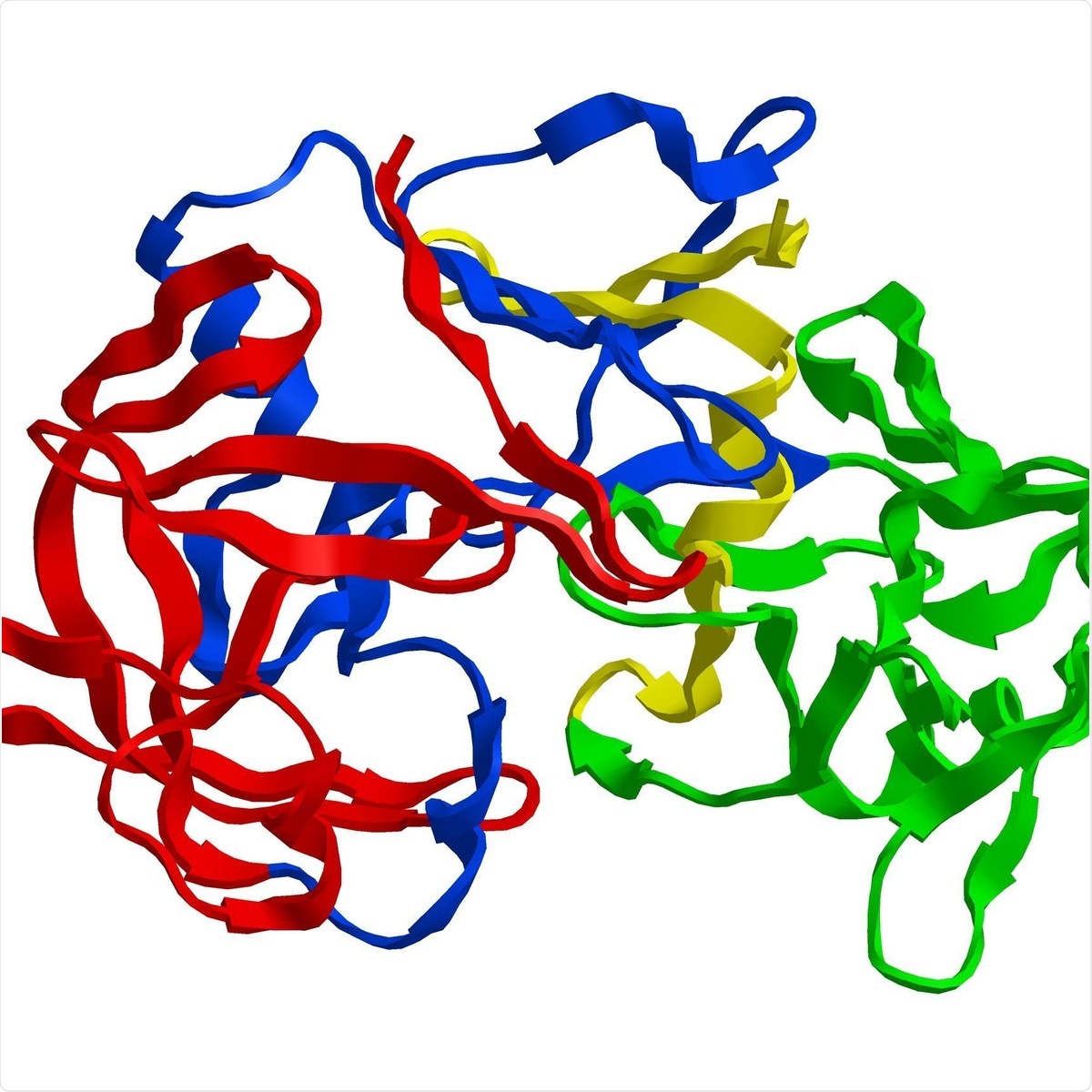
Molecular structure of digestive protein pepsin, enzyme that breaks down proteins into smaller (protease). Image Credit: Raimundo79 / Shutterstock.
Proteases also play pivotal roles in the biochemical and physiological processes throughout the body.
Furin, which was officially identified in 1990, catalyzes a simple biochemical reaction – the proteolytic maturation of proprotein substrates in the secretory pathway. The protease has an important role in homeostasis, as well as diseases ranging from Alzheimer's disease and anthrax to Ebola fever, cancer, diabetes, obesity, and hypertension.
Furin and COVID-19
Coronaviruses (CoVs) contains four structural proteins, including the Spike (S), Membrane (M), Envelope (E), and Nucleocapsid (N). Spike, a trimeric glycoprotein of coronaviruses, mediates the coronaviruses' binding to the host cell's surface-specific receptors.
The Spike protein plays a key role in the early stages of viral infection, with the S1 domain responsible for receptor binding. Meanwhile, the S2 domain mediates membrane fusion.
The S glycoprotein must be cleaved by cell proteases to enable exposure of the fusion sequences, which is needed for cellular entry. The nature of cell proteases that cleave the S glycoprotein differs according to the type of coronavirus.
For instance, the severe acute respiratory syndrome coronavirus (SARS-CoV), S glycoprotein is uncleaved upon virus release from cells but is likely cleaved during virus entry into a cell. This is the agent that was responsible for the SARS outbreak that occurred in China in 2002.
In contrast, the Middle East respiratory syndrome coronavirus (MERS-CoV), S glycoprotein contains a furin cleavage site and is processed by the intracellular proteases upon exit from the cell. The MERS outbreak emerged in Saudi Arabia in 2012.
Meanwhile, the Spike glycoprotein of the newly emerged SARS-CoV-2 – the causative pathogen for COVID-19 – contains a furin cleavage complex (FCC). The modified S glycoprotein can interact with the cell surface receptor angiotensin-converting enzyme 2 (ACE2), which is the specific receptor found in human cells, particularly epithelium, that the virus utilizes to gain entry. The S1 or receptor-binding domain contacts with ACE2, which is facilitated by a furin cleavage.
Recent research has shown that the S protein of SARS-CoV-2 is between 10 and 20 times more likely to bind to human ACE2 than the S protein of previous coronaviruses. This means that SAR-CoV-2 is significantly more infectious than both SARS and MERS.
Viral hijacking of furin protease
In the current study, Dr. Fitzgerald noted that SARS-CoV-2 uses endogenous furin to cleave the S protein in the trans-Golgi network right after virion assembly. The mechanism separates furin from other virally hijacked proteases, which may increase the pathogenicity of SARS-CoV-2.
The presence of the FCC allows the virus to spread systematically and cause higher rates of severe disease and death. Furin is present in most tissues and is highly expressed in the lungs, which may explain how the virus gains entry into the respiratory tract and causes infection.
The study explored how the potential that baseline inflammation contributes to a delayed response from the immune system. Also, furin may hold the key to a better understanding of why there are virus-initiated immune responses and an influence of comorbidities on COVID-19 severity.
Furin and comorbidities
The United States has been overwhelmed with the spread of SARS-CoV-2. More than 1 in 3 Americans are also thought to have cardiometabolic diseases, which are known as comorbidities to COVID-19.
Dr. Fitzgerald noted that the presence of elevated furin levels seen in this population makes them vulnerable to SARS-CoV-2 entry and replication. They are more susceptible to being infected with SARS-CoV-2 and more likely to experience severe complications as it spreads rapidly throughout the body.
Further, furin activates several peptides that may drive the development of COVID-19 disease. First, furin facilitates the renin-angiotensin-aldosterone system (RAAS) by stimulating the prorenin receptor. As a result, vasoconstrictor angiotensin is formed, and aldosterone is secreted, which can cause hypokalemia.
Hypokalemia and RAAS interference through ACE2 are seen in COVID-19.
Some COVID-19 patients experience coagulopathy and hypoxia, which involves the clotting factor VIII and the von Willebrand factor. Furin is needed in the activation of the clotting factor VIII.
All these mechanisms contribute to developing severe symptoms of COVID-19. Severe hypoxia being a hallmark finding in severe COVID- 19 cases.
Therapeutic target
Furin may therefore act as a therapeutic target for COVID-19 treatment. Furin inhibition may help in treating severely ill patients.
Heparin is a furin inhibitor and has an accepted risk-benefit ratio. Since some patients with severe COVID-19 experience the risk of coagulopathy, heparin use has been linked to lower mortality in hospitalized patients.
Also, hypoxia induces furin expression as well as all 3 FUR gene promoters harbor binding sites for hypoxia-inducible factor-1 (HIF-1). Berberine, which is an HIF-1 inhibitor, maybe a potential treatment for COVID-19 patients.
Lastly, lifestyle modification among high-risk patients and those with comorbidities may help reduce furin levels and baseline inflammation. Maintaining a healthy weight and lifestyle can hamper viral entry and replication.
"Addressing comorbidities (and associated elevated furin levels) through diet, lifestyle modifications, and pharmacologic management is a logical strategy for reducing COVID-19 pathogenicity. Natural and pharmacologic furin inhibitors may prove highly useful to inhibit viral entry and propagation," the researcher concluded in the study.