Many coronavirus 2019 (COVID-19) recovering patients who have been affected by the severe acute respiratory coronavirus 2 (SARS-CoV-2) infection can experience persistent symptoms which can last beyond 4 weeks. This can be known as ‘long COVID’ and can include a broad range of symptoms, such as breathlessness and fatigue and this can overlap with post-intensive care syndrome (PICS).
PICS can include a wide variety of physical, psychological, and cognitive symptoms which can affect 25% of critically ill survivors, who experience fatigue, posttraumatic stress, and muscle weakness. This syndrome can last up to 5 years and can affect the readmission rates of patients who are struggling to recover from fatigue-related illnesses such as COVID-19.
The significance of fatigue in COVID-19 infections
Fatigue has been described as the most common symptom of ‘long-COVID’ within community and hospital-managed acute COVID-19 infections, with this symptom being reported in 97.7% of community-managed cases. This symptom has been reported to last over 28 days in these cases, while also being recorded in 83% and 98% of UK and Chinese patients, respectively, more than 3 months after being admitted into hospital for SARS-CoV-2.
Recent studies have suggested that fatigue may be a higher consequence for patients that required invasive mechanical ventilation (IMV); with the ranges of fatigue being found in ICU-recovered patients from 13.8% to 80.9%, it is a significant symptom that requires a closer look.
A UK-based study has aimed to characterize the prevalence and severity levels of fatigue as a long-lasting symptom post-COVID-19 in patients who were ICU-survivors, compared to patients who experienced a milder form of the infection. This study aims to explore these findings to effectively identify which groups of the population are at more risk of having longer-lasting effects of the 2019 coronavirus.
A pre-print version of the paper is available on the medRxiv* server, while the article undergoes peer review.
The study
The researchers of this study undertook a secondary analysis of two prospectively collected datasets, including a COVID-19 cohort: International Severe Acute Respiratory Infection Consortium Coronavirus Clinical Characterisation Protocol - United Kingdom (ISARIC-4C CCP-UK) and a pre-pandemic cohort: Evaluation of a Rehabilitation Complex Intervention for Patients Following Intensive Care Discharge (RECOVER) trial.
The CCP-UK study included 355 COVID-19 patients, with 27.5% having received IMV, while 240 patients were included in the pre-pandemic RECOVER study with 35% of patients receiving IMV.
The pre-pandemic cohort was used as a baseline for this comparison with the COVID-19 IMV-patients, and the potential associations were explored in both of these groups.
These studies utilized questionnaires to collect the data from patients as well as some face-to-face or telephone assessments at times. The primary outcome from the secondary analysis was patient-reported fatigue severity with the outcomes being, severe fatigue, breathlessness, and measures of related quality of life.
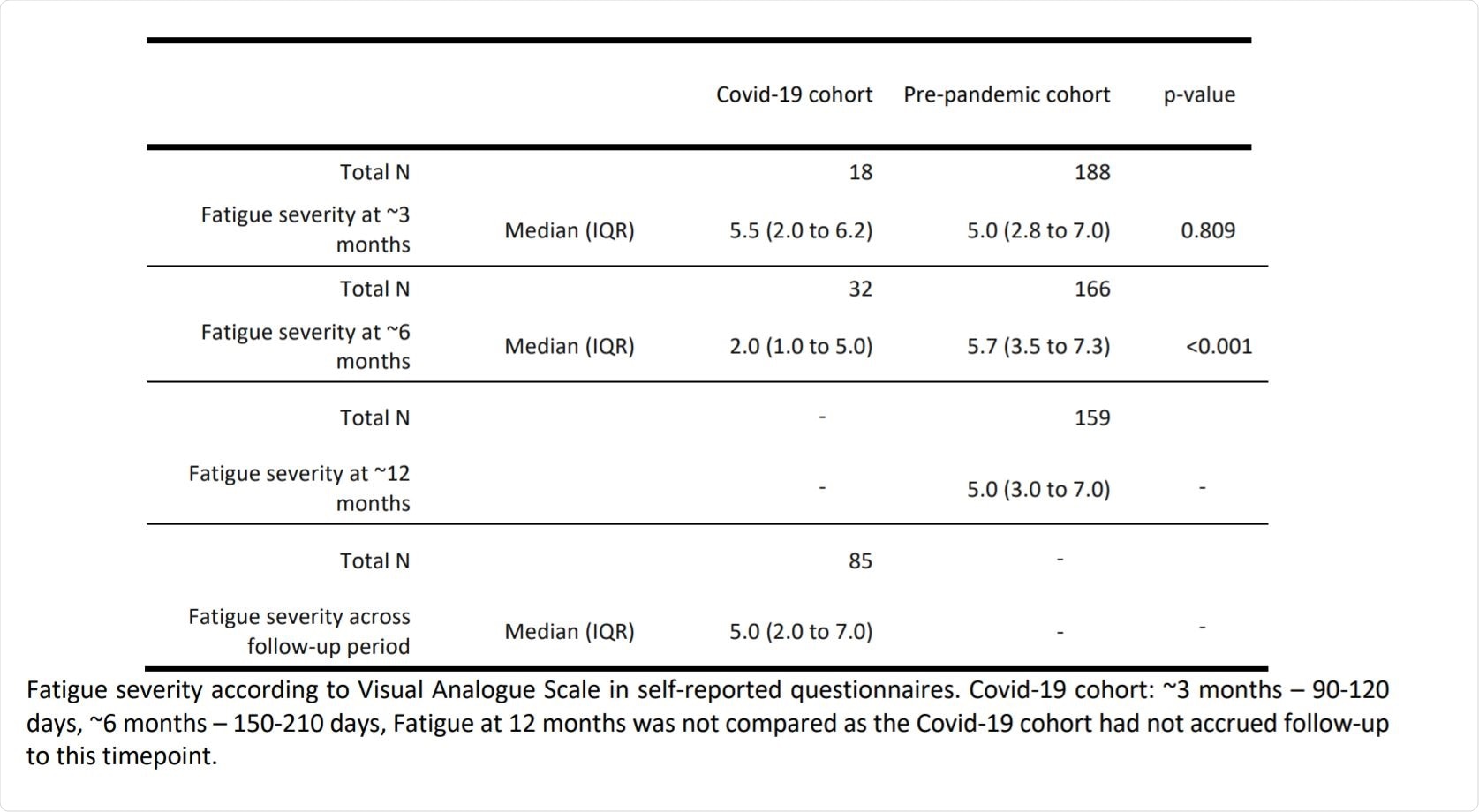
Study Findings. Image Credit: https://www.medrxiv.org/content/10.1101/2021.06.15.21258879v1.full.pdf

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Findings
The researchers had found a high prevalence and severity of persistent fatigue that was reported in both critical and mild-manifesting COVID-19 ventilated patients after they had been discharged. After 6 months post COVID-19, patients who had been ventilated for this infection had reported significantly less fatigue than those patients who had been ventilated for other illnesses.
During the investigating of both studies, women under the age of 50-years-old in the CCP-UK study had experienced more fatigue and health-related problems compared to other patients. This result differed from the pre-pandemic IMV patient study group, where there was no bias in results for the different sexes included.
Both of these research groups had been found to have levels of severe fatigue and long-lasting side effects which affected their quality of life; however, with differences at the 6-month period in women who may have experienced a more severe form of this symptom, this group could be seen as being a potential target for risk. While younger counterparts of infected patients had survived the illness to a higher degree, younger female survivors had experienced fatigue and a harder quality of life than other COVID-19 IMV patients.
The results of this UK analysis illustrated that those who had survived COVID-19 infections the most consisted of younger patients with fewer comorbidities. For this group of individuals, less long-lasting fatigue was reported at 6-months after having a critical experience with SARS-CoV-2. It was found that these patients had also been targeted for early discharge from the hospital due to the need for ICU beds to focus on the survival of patients at any functionality level rather than the rehabilitation of each patient till they had reached an optimum health level.
There may also be other variables that can affect fatigue levels including mental health and disorders such as depression and anxiety which may be experienced to a higher level for patients with this infection due to the isolation and hardships they had faced during this time.
This UK analysis has enabled a deeper insight into the lasting effects of COVID-19 infections and can aid with further research into the discrepancies faced by certain at-risk groups that experience fatigue and other health-related problems which affect the overall quality of life post-COVID-19.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Pauley, E.E., Drake, T.M., Griffith, D., Lone, N.I., Harrison, E.M., Baillie, J.K., Scott, J.T., Walsh, T.S., Semple, M.G. and Docherty, A.B. (2021). Recovery from Covid-19 critical illness: a secondary analysis of the ISARIC4C CCP-UK cohort study and the RECOVER trial. https://doi.org/10.1101/2021.06.15.21258879
- Peer reviewed and published scientific report.
Pauley, Ellen, Thomas M Drake, David M Griffith, Louise Sigfrid, Nazir I Lone, Ewen M Harrison, J Kenneth Baillie, et al. 2021. “Recovery from Covid-19 Critical Illness: A Secondary Analysis of the ISARIC4C CCP-UK Cohort Study and the RECOVER Trial.” Journal of the Intensive Care Society, October, 175114372110522. https://doi.org/10.1177/17511437211052226. https://journals.sagepub.com/doi/10.1177/17511437211052226.