In a recent study published in the journal Science Translational Medicine, researchers investigated the impact of aging on immune response, viral dynamics, and nasal microbiome in 1031 hospitalized coronavirus disease 2019 (COVID-19) patients, using advanced profiling techniques to understand age-related differences in disease severity and immune function.
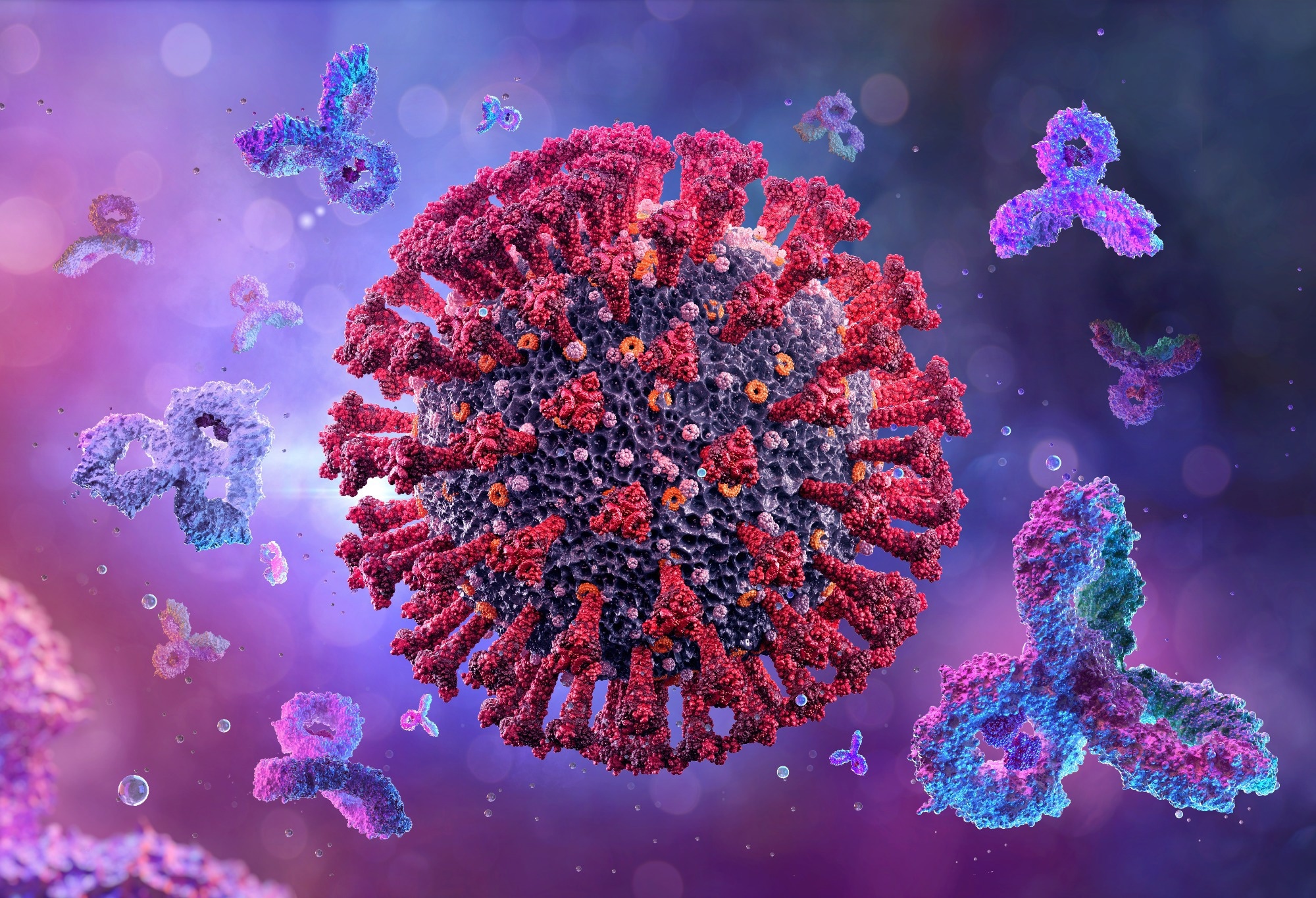 Study: Host-microbe multiomic profiling reveals age-dependent immune dysregulation associated with COVID-19 immunopathology. Image Credit: Corona Borealis Studio / Shutterstock
Study: Host-microbe multiomic profiling reveals age-dependent immune dysregulation associated with COVID-19 immunopathology. Image Credit: Corona Borealis Studio / Shutterstock
Background
Age is a significant risk factor for severe COVID-19 outcomes, with older adults facing drastically higher risks of complications and mortality than younger individuals. Despite high vaccination rates, older adults are still profoundly vulnerable. Aging correlates with elevated levels of inflammatory cytokines, like interleukin-6 (IL-6), which are critical markers of COVID-19 severity, hinting at a link between aging and disease pathophysiology. Studies show that aging dampens both innate and adaptive immune responses, including reduced type I interferon (IFN) production. Additionally, older adults show enhanced inflammatory responses and impaired immune signaling when infected with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Further research is needed to fully understand the complex interactions between aging, immune response variations, and COVID-19 severity to improve treatment strategies and outcomes for older populations.
About the study
The present study utilized data from 1,031 participants enrolled in the IMmunoPhenotyping Assessment in a COVID-19 Cohort (IMPACC) observational cohort, which involved 20 hospitals across 15 medical centers in the United States from May 5, 2020, to March 19, 2021. It involved hospitalized individuals with reverse transcription polymerase chain reaction (rt-PCR) confirmed SARS-CoV-2 infections, displaying typical COVID-19 symptoms. Blood and respiratory tract samples were collected within 72 hours of hospitalization, following a standardized protocol across participating institutions. Ethical approval was granted under the public health surveillance exception, with participant consent for follow-up involvement and data usage.
Statistical analysis was performed using R software. Initial assessments were done within 72 hours of hospital admission, followed by longitudinal evaluations at subsequent visits. Data analysis applied various statistical methods depending on the data type and required adjustments for factors like age, sex, and baseline disease severity. For longitudinal studies, age groups were divided into quintiles and analyzed for changes in viral abundance and immune response, employing linear and generalized additive models to account for the observed non-linear patterns. All p-values were adjusted using the Benjamini-Hochberg method, considering results statistically significant at p < 0.05.
Study results
The study involved analyzing blood and nasal swab specimens from 1,031 vaccine-naïve adults hospitalized with COVID-19. These participants were part of the IMPACC cohort, sourced from 20 hospitals across the United States. They were categorized into five age quintiles, ranging from 18 to 96 years, with each group comprising between 187 and 223 individuals. Samples were collected at the time of hospital admission and during up to five follow-up visits. The distribution of ages showed that older individuals were often more severely affected by the disease, evident in both the initial severity of symptoms and the outcomes, including mortality.
At the initial hospital visit, typically within 72 hours of admission, a range of diagnostic assays was conducted. These included transcriptional profiling of peripheral blood mononuclear cells (PBMCs) and nasal swabs, serum inflammatory protein profiling, whole blood mass cytometry (CyTOF), nasal metatranscriptomics, and SARS-CoV-2 antibody (Ab) assays. A significant finding from these initial tests was that older adults displayed higher viral loads and experienced delayed viral clearance compared to younger patients. Moreover, age-related differences in immune cell populations were noted, with older adults showing higher proportions of various monocyte subtypes and activated T cells but lower levels of naïve T and B cells.
The study's longitudinal analysis revealed that these differences persisted over time, affecting viral load dynamics, antibody titers, and immune response. Specifically, the eldest participants not only retained high levels of the virus longer but also showed more significant fluctuations in antibody levels over time. Additionally, immune cell analysis by CyTOF highlighted that with advancing age, certain immune cell types, including different monocyte classes and differentiated natural killer cells, increased, suggesting shifts in immune system composition and function with age.
Changes in cytokine and chemokine levels measured in the participants' serum further underscored the impact of aging on the immune response. Older individuals showed elevated levels of inflammatory markers at hospital admission, which were linked to more severe disease outcomes.
Moreover, the analysis extended to the nasal microbiome and upper respiratory gene expression, revealing age-associated changes in the microbial composition and host gene activity. Changes in Toll-like receptor signaling and other immune pathways were evident, suggesting that older adults experience different immune modulations, possibly influencing their susceptibility to severe outcomes.