Why do we feel listless when we are recovering from an illness? The answer is, apparently, that low-grade chronic inflammation interferes with the dopaminergic signaling system in the brain that motivates us to do things.
The research carried out at Emory University explains the links between the reduced release of dopamine in the brain, the motivation to do things, and the presence of an inflammatory reaction in the body. It also presents the possibility that this is part of the body’s effort to optimize its energy expenditure during such inflammatory episodes, citing evidence gathered during their study.
The authors also published an experimental framework based on computational tools, devised to test the theory.
The underlying hypothesis is that the body needs more energy to heal a wound or overcome an infection, for instance, both of which are associated with low-grade inflammation. To ensure that energy is available, the brain uses an adaptive technique to reduce the natural drive to perform other tasks which could potentially drain away the energy needed for healing. This is essentially a recalibration of the specialized reward neurons in the motivation center of the brain, so that ordinary tasks no longer feel like they’re worth doing.
According to the new study, the mechanism of this recalibration is immune-mediated disruption of the dopamine pathway, reducing dopamine release.
The computational technique published by the scientists is designed to allow experimental measurements of the extent to which low-grade inflammation affects the amount of energy available, and the decision to do something based on the effort needed. This could allow us to better understand why and how chronic inflammatory states cause a lack of motivation in other disease conditions as well, including schizophrenia and depression.
Andrew Miller, co-author of the study, says, “If our theory is correct, then it could have a tremendous impact on treating cases of depression and other behavioral disorders that may be driven by inflammation. It would open up opportunities for the development of therapies that target energy utilization by immune cells, which would be something completely new in our field.”
It is already known that immune cells release cellular signaling molecules called cytokines, which affect the functioning of the dopamine-releasing neurons in the area of the brain called the mesolimbic system. This area enhances our willingness to work hard for the sake of a reward.
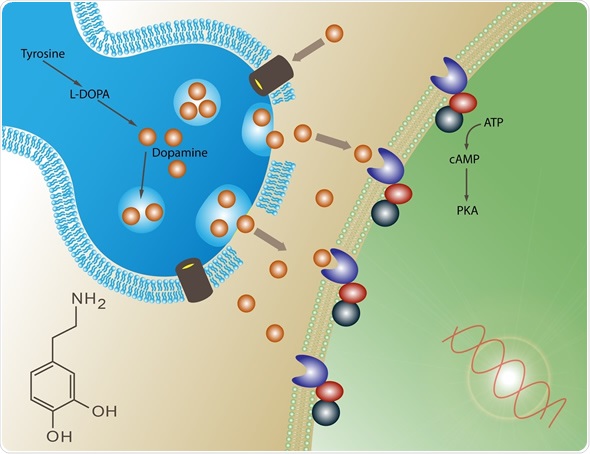
Image Copyright: Meletios, Image ID: 71648629 via shutterstock.com
Recently, it was discovered that immune cells also enjoy a unique capability to shift between various metabolic states, unlike other cells. This could affect cytokine release patterns in such a way as to signal the brain to conserve available energy for the use of the immune system.
These facts were the foundation of the new hypothesis, which explains it in terms of evolutionary adaptation. In the hypothetical early environment, the immune system, faced with abundant microbial and predatory challenges, needed tremendous amounts of energy. It therefore had its own mechanism to signal other body systems, via the mesolimbic dopamine system, to control the use of energy resources during periods when the organism was undergoing severe or sudden stress.
Modern life is relatively soft and less challenging. With less physical activity, low-grade inflammation is chiefly due to factors such as obesity, chronic stress, metabolic syndrome, aging and other lifestyle illnesses. This could mistakenly cause the mesolimbic dopamine neurons to produce less dopamine. Lower dopamine levels in turn decrease the motivation for work, by reducing the perception of reward while increasing the perception of effort involved. This ultimately conserves energy for use by the immune system.
Previous studies by Miller as well as other scientists have shown that a high level of immune functioning in association with low levels of dopamine and reduced motivation characterizes some cases of schizophrenia, depression and certain other mental health conditions.
The scientists do not think these disorders are caused by the low-grade inflammation, but that some people who have these illnesses are hypersensitive to immune cytokines. This could in turn cause them to lose motivation for daily living.
The scientists are currently performing a clinical trial on people with depression, to test the theory using the computational framework.
Source: Treadway M. T. et al., (2019). Can’t or Won’t? Immunometabolic Constraints on Dopaminergic Drive. Trends in Cognitive Sciences. https://doi.org/10.1016/j.tics.2019.03.003