A new report by the World Health Organization (WHO) shows that 4.5 million deaths could be prevented by 2030, and 26 million beyond that, if 67 countries in the low- and middle-income bracket invest $6 billion a year towards abolishing hepatitis. Hepatitis is a completely preventable and treatable illness at present, and in fact, hepatitis C is completely curable.
Viral hepatitis is classified as hepatitis A, B, C, D and E, with 95% or more of deaths being due to chronic hepatitis B and C. Hepatitis A and E are typically mild self-limited infections. Hepatitis D occurs only in association with hepatitis B, but accelerates cirrhosis and cancer of the liver following the latter infection. Hepatitis E is usually mild but if acquired in late pregnancy, can kill up to a quarter of pregnant women, as well as causing increased fetal loss rates.
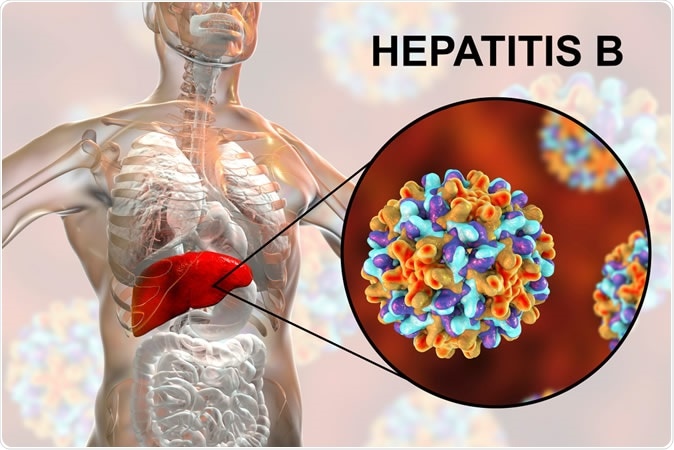
Liver with Hepatitis B infection highlighted inside human body and close-up view of Hepatitis B Viruses. 3D illustration - Illustration Credit: Kateryna Kon / Shutterstock
Hepatitis A
Hepatitis A is food-borne or transmitted via direct contact. It is among the leading foodborne infections, causes cyclic epidemics, and can cause significant illness and loss of productivity, but only about 0.5% of deaths. Prevention includes food and water sanitation, hand washing, and vaccination for high-risk individuals like travelers to epidemic countries, those having sex with male homosexuals and injectable drug users.
Hepatitis B
Hepatitis B and C infections, singly or together, affect about 325 million people, killing almost 1.5 million a year. Chronic infection is associated with high rates of cancer and cirrhosis of the liver in both adults and children, but especially the latter. 12% of cases occur in the Western Pacific and African regions.
Of about 255 million chronic hepatitis B patients, only about 10% knew their infection status in 2016. Less than 5 million (17%) were treated, while 1.1 million were newly diagnosed with chronic hepatitis B. Over.
90% of new hepatitis B infections occur from mother to child or in young children. Almost all of these become chronic, compared to the less than 5% in healthy adults. Other pathways for hepatitis B/C infections include unsafe needles drugs, tattoos, acupuncture), unprotected sex with male homosexuals or infected partners, and infected body fluids (health care workers). Hepatitis B immunization within 24 hours of birth is the best way to prevent it, providing at least 20 years of protection and perhaps lifelong immunity in 95% of vaccinees. Ensuring blood and blood component safety is another preventive strategy. Hepatitis B prevention also prevents hepatitis D.
Diagnosis is by means of blood testing for the HbsAg, IgM antibody, and HbeAg molecules in various combinations. Chronic hepatitis B infection is suppressed by lifelong treatment with tenofovir or entecavir, with the former costing only $32 a year in generic form. Both are now freely available worldwide.
Hepatitis C
Hepatitis C is acquired by contact with blood or body fluids, including injections, needlesticks, unsafe blood and blood products, and high-risk sex.
Of the 71 million chronic hepatitis C cases in 2017, only 1 in 5 knew their infection status and only 15% obtained curative treatment. Over 1.7 million newly diagnosed cases occurred, with 400 000 deaths in 2017. 70% or more of infections turn chronic. 95% or more of cases can be cured in three months, but few know about or have access to treatment.
Diagnosis is via anti-HCV antibody and anti-HCV RNA testing. Prevention includes needle safety, blood safety, hand hygiene, and protected sex. Secondary prevention to contain its spread includes hepatitis A and B vaccination, antiviral therapy which is now only about $40 per cure in low-and middle-income countries, and monitoring for chronic infection.
World Hepatitis Day
The international WHO event day called the World Hepatitis Day on July 28 was held in Pakistan this year. It is meant to educate and raise awareness of this deadly and disabling condition. It honors the birthday of Nobel laureate Baruch Bloomberg, who discovered the hepatitis B virus as well as tests and vaccines for it.
Currently, medical care is inaccessible for 8 out of 10 people with hepatitis, including preventive, diagnostic and curative care. This has fueled the call for governments to invest largely into this sector in view of the high cost-effectiveness. For less than $60 billion new hepatitis cases can be reduced by an astounding 90% while preventing 65% of deaths.
Under the 2019 banner, “Invest in eliminating hepatitis”, the WHO is emphasizing the possibilities offered by the low cost of current hepatitis diagnosis and treatment, calling upon member countries to make appropriate investments to achieve this goal.
While the vast majority of its 194 members have already prepared plans to achieve this milestone, only about 60% have actually budgeted for this. To help assess the cost-benefit ratios of the new initiatives, WHO has also released online calculators.
Some political leaders have already responded, such as in India, for instance, which has declared its new policy of providing free diagnostic and treatment facilities for hepatitis C and B under its universal health coverage plan. Pakistan has also obtained inexpensive drugs for hepatitis C cure, at below $40. As a result, healthcare costs in relation to hepatitis C will actually decline despite the free testing and treatment plan, within just 3 years.