Children were relatively spared during the first wave of coronavirus disease 2019 (COVID-19). More recently, an increasing number of children are falling ill as a result of the spread of newer variants of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).

Study: Health care use up to 6 months after COVID-19 in 700.000 children and adolescents: a pre-post study. Image Credit: L Julia / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Long-term health care following COVID-19
Adults with COVID-19 are known to present with a wide range of symptoms, the most common of which includes chest tightness, shortness of breath, or cardiac symptoms. These symptoms typically remain evident between 3 and 6 months after the initial infection.
Current research indicates that the persistence in these complaints commonly occurs in adults recovering from severe COVID-19. Still, several other studies have demonstrated that even asymptomatic or mild illness can be followed by long-term complaints.
Together, this points to a significant increase in the utilization of healthcare services by these patients for months after their initial illness. The situation is less clear with children. In rare cases, children can develop multisystem inflammatory syndrome in children (MISC); however, their long-term prognosis following recovery from SARS-CoV-2 remains unknown.
Earlier studies on COVID-19 in children have been small and mainly include children with moderate-to-severe COVID-19. In order to predict and prepare for the healthcare needs of the pediatric population affected by COVID-19, wider studies based on this specific patient population are necessary. To this end, studies should aim towards understanding the scale and duration of long-term complications, as well as the age at which these complications are most likely to occur.
Study details
The current study used data from an emergency preparedness register established by the Norwegian Institute of Public Health (NIPH). This register includes all polymerase chain reaction (PCR) tests for the virus conducted in Norway with the test date and result. The researchers restricted their analysis to the period between August 1, 2020 to February 1, 2021, as testing was widespread by this time.
The test population excluded severely ill children with COVID-19. Notably, children with chronic conditions who would be more frequently tested, such as before attending hospitals for routine or specialist visits, were not included in the study. All other children were classified into those who tested positive or negative for COVID-19, as well as children who were never tested for the virus.
The difference in the rate of healthcare use before and after a positive/negative PCR test, as well as untested children (the latter being assigned a random test date matching the distribution of the other two categories), was used to assess the impact of the illness.
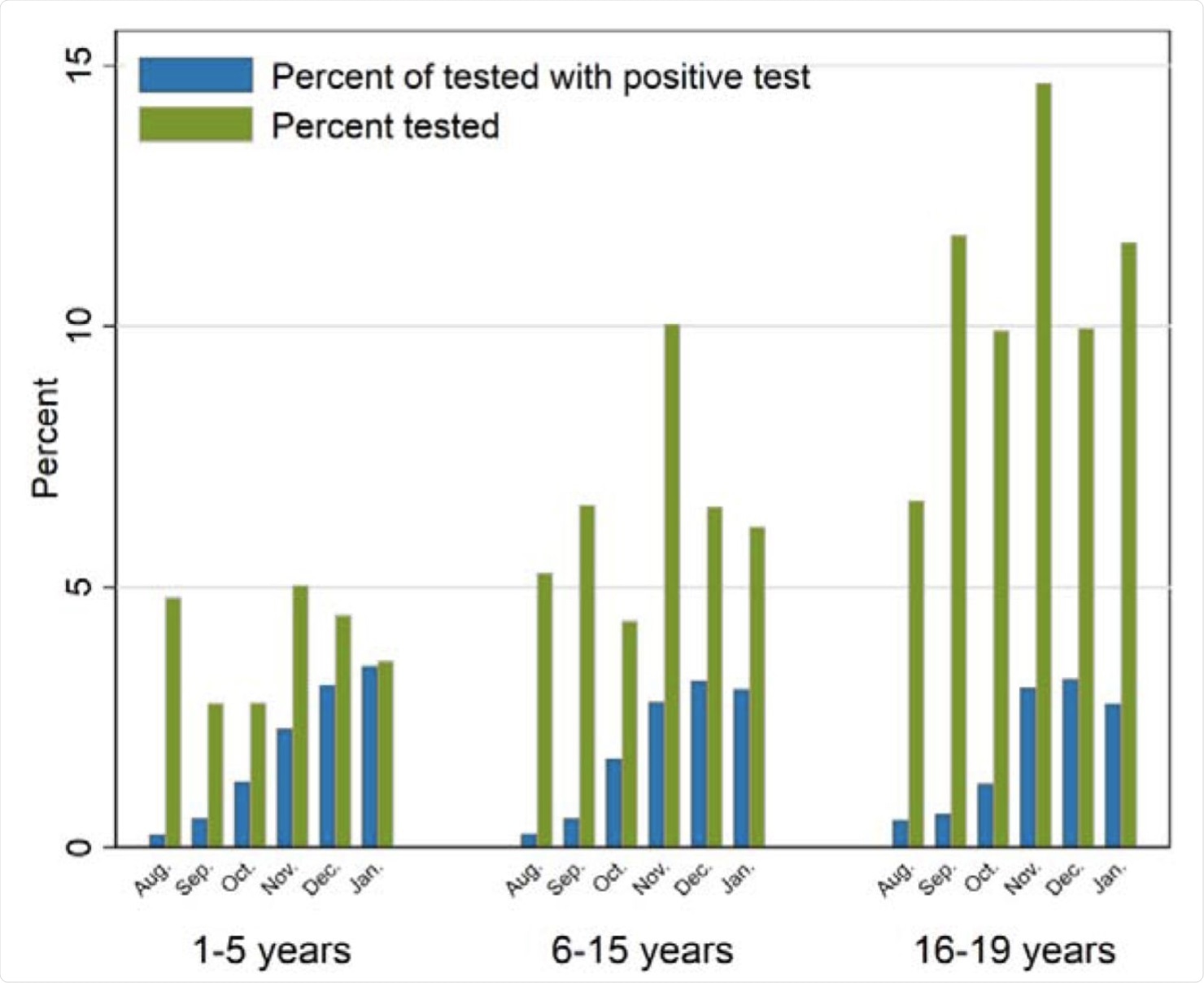 Percentage of the sample being tested for SARS-CoV-2 in PCR test by month (August to December 2020, and January 2021), and percentage of the tested who tested positive for SARS-CoV-2 per month, by age group.
Percentage of the sample being tested for SARS-CoV-2 in PCR test by month (August to December 2020, and January 2021), and percentage of the tested who tested positive for SARS-CoV-2 per month, by age group.
About 760,000 of the 1.3 million children in Norway were included in this follow-up. Approximately 300,000 had been tested, of which just over 10,000 were positive, which amounts to about 1.3% of the study population. COVID-19 positive children were categorized into those aged 1-5, 6-15, and 16-19 years.
Testing was lowest for the youngest group of children, whereas positive COVID-19 cases made up a similar percentage among all age groups. Norwegian-born children were found least likely to be positive.
Increased primary care visits in test-positive children
Primary care use by children who tested positive for COVID-19 significantly increased from 3% before testing to 41% during the week of testing. This use of primary healthcare services then reduced to 16% by week 4. Thereafter, the COVID-19 positivity rate remained constant at about 4% for up to three months, and at 3% for up to six months.
The same patterns were noted within specific age groups. Among the children who tested negative, the rise in primary healthcare use was both less steep and less sustained. Notably, there no detectable difference in primary care use was found in the children who were never tested for COVID-19.
The most frequent complaints were respiratory and general symptoms.
Positives vs. negatives
The greatest relative increase in COVID-19 cases was seen over the first four weeks, during which children aged 1-5 years who tested positive had a 325% increase in primary care use as compared to those who tested negative. The increase was 434% for those between 6-15 years, and 360% for the oldest children who were between the age of 16 and 19 years.
At 5-8 weeks after the test, primary healthcare use remained elevated by up to a fifth among children up to 15 years of age who tested positive as compared to those who tested negative for COVID-19. COVID-19 positive children continued to show 26% (among those aged 1-5 years) and 15% (for those aged 6-15 years) higher positivity rates in the third month.
Among the pre-schoolers who tested positive, a 14% increase in primary healthcare use continued to be seen 3-6 months following the initial infection, which was comparable to 8% for the oldest test-negative children. Those aged 6-15 years did not show any excess healthcare use during this period.
Specialist care was not increased among children who tested positive at any time point, compared to those who tested negative for COVID-19.
Positives vs untested
Compared to untested children, the differences were even more striking. Primary care use among COVID-19 positive children increased by approximately 700% over the first four weeks after their test, while the relative increase was almost a thousand times higher among those aged 6-19 years.
The increase continued to be seen by 33-50% over all age groups, up to three months post-test.
Untested children aged 16-19 years showed a 32% increase in the long-term use of primary healthcare, relative to the positives.
What are the implications?
This earliest large-scale study of long COVID in a general pediatric cohort shows that it is probably limited to symptoms that are treated at the primary care level. The most persistent symptoms, up to six months, were in identified pre-schoolers, relative to those who tested negative.
This could be explained by the known predisposition of respiratory symptoms to linger after viral infections affecting the airway occur in very young children.
Overall, younger children appeared to require more visits to general practitioners post-COVID-19, predominantly in the first four weeks but continuing at lower levels for up to six months. Those between the ages of 6-15 and 16-19 years had more frequent visits for only up to three months after recovering from COVID-19. Specialist care was not accessed more frequently by any age group.
“The findings suggest that COVID-19 does not lead to severe long-term health problems in children and adolescents, at least not problems that require follow-up by (specialist) health care services.”
This type of study may help decide whether children should be vaccinated against the virus and whether viral spread should be contained by social distancing and other measures after all adults are vaccinated.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Magnusson, K., Skyrud, K. D., Suren, P., et al. (2021). Health care use up to 6 months after COVID-19 in 700.000 children and adolescents: a pre-post study. medRxiv preprint. doi:10.1101/2021.06.02.21258211. https://www.medrxiv.org/content/10.1101/2021.06.02.21258211v1.
- Peer reviewed and published scientific report.
Magnusson, Karin, Katrine Damgaard Skyrud, Pål Suren, Margrethe Greve-Isdahl, Ketil Størdal, Doris Tove Kristoffersen, and Kjetil Telle. 2022. “Healthcare Use in 700 000 Children and Adolescents for Six Months after Covid-19: Before and after Register Based Cohort Study.” BMJ, January, e066809. https://doi.org/10.1136/bmj-2021-066809. https://www.bmj.com/content/376/bmj-2021-066809.