Sponsored Content by Cerba ResearchReviewed by Louis CastelJan 28 2025
Next-generation flow (NGF) cytometry offers a number of advantages when used in the immunophenotyping of plasma cells in CAR+ T-cell clinical trials.
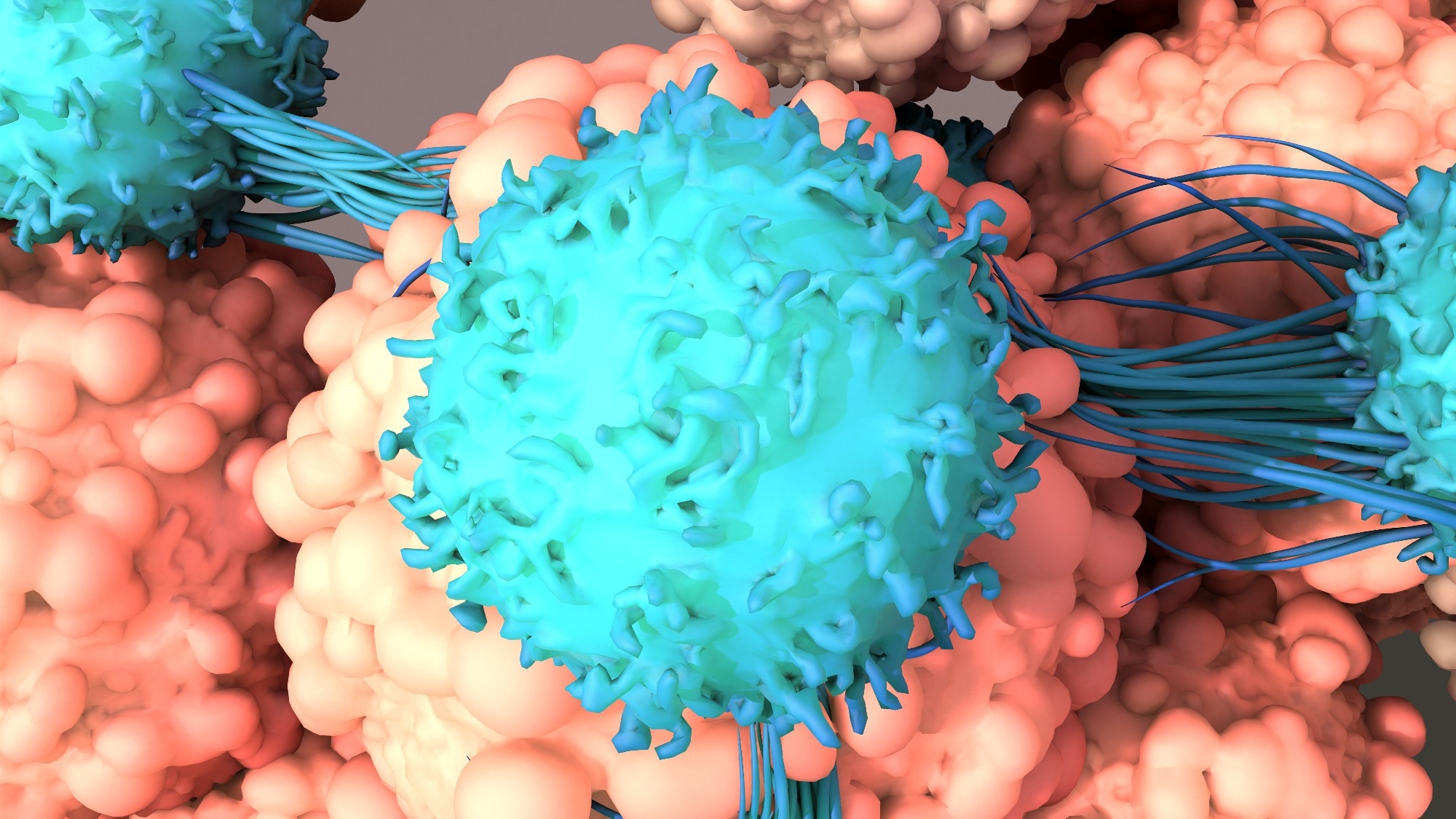 Image Credit: Design_Cells/Shutterstock.com
Image Credit: Design_Cells/Shutterstock.com
Next-generation flow cytometry benefits from standardization at each step of the process, from sample preparation and data acquisition through to reporting. This method also benefits from a wide selection of backbone markers and the ability to achieve higher levels of sensitivity than first-generation flow cytometry.
Next-generation flow cytometry is conducted at the beginning of CAR+ T-cell therapy in order to identify and quantify malignant plasma cells in the bone marrow and investigate the presence of antigens. This may be done at diagnosis or as part of the screening process.
Immunotherapeutic drugs such as CAR+ T-cell therapy will then be used to target antigens on the surface of plasma cells. NGF is also important during follow-ups to treatment because targeted therapy has the potential to induce phenotypical changes in plasma cells and alter the expression of the targetable antigens.
The therapy’s efficacy can be evaluated by confirming the disappearance of monoclonal plasma cells. NGF can also be used to evaluate MRD, which is an increasingly critical consideration due to its potential use as a marker for progression-free survival and overall survival in clinical trials.
Immunophenotyping of plasma cells in multiple myeloma
Immunophenotyping of plasma cells in patients with multiple myeloma is performed using a specific set of recommended markers. Plasma cell populations can be identified based on the expression of CD45, CD38, and the more plasma cell-specific marker CD138. These markers allow plasma cells to be classified as either normal or abnormal.
The next step in this process involves evaluating the expression of another set of plasma cell-characterizing markers. Malignant plasma cells are typically either CD19 negative and CD56 positive, and these may also exhibit a weaker or absent expression of CD27 and CD81.
Very few multiple myeloma patients exhibit CD117 expression on malignant plasma cells, but this should still be considered.
The final stage of this process involves the use of intracellular staining to investigate the monoclonality of the malignant plasma cells for kappa and lambda light chains. This assessment should, ideally, lead to the useful discrimination of both normal and abnormal plasma cells.
A number of other markers may be suitable for use in multiple myeloma panels alongside the currently recommended markers; for example, markers such as CD28 and CD200 are useful predictors of disease progression.
CD138 is known to be a relatively unstable marker, and its expression diminishes 8-24 hours after the sample has been acquired. If analysis is anticipated to be delayed, it may be prudent to add a more stable marker to the panel, such as CD319.
Acknowledgments
Produced from materials originally authored by Ans De Beuckelear, Ph.D., and Rowan Claeys from Cerba Research.
About Cerba Research
For over 35 years, Cerba Research has been setting the industry standard for exemplary clinical trial conduct. Today, across five continents, with a focus on precision medicine, we are changing the paradigm of the central lab’s role in complex clinical research.
From protocol inception through development and to market, our passionate experts deliver the highest quality specialized and personalized laboratory and diagnostic solutions. Partner with us for the most efficient strategy to actualize your biotech and pharmaceutical products sooner and improve the lives of patients worldwide.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.