A frequently reported fact in the drug discovery and development industry is that approximately 90 % of drug candidates reaching clinical trials fail, with even higher amounts discarded before arriving at the clinic.
Recently, a market survey of large Pharma companies and mid-sized Biotechs highlighted cost and efficacy as primary concerns during drug development, demonstrating the impact of failed drugs. Lack of efficacy is the predominant cause of these failures with unexpected adverse effects in patients second.
More translatable data between the preclinical and clinical phases of drug discovery and development is required to address the financial uncertainty that surrounds the process.
The NAM revolution
A wide range of preclinical tools are available to scientists to evaluate drug safety and efficacy, including basic in vitro 2D/3D cell culture assays and in vivo animal models.
The former is convenient and scalable, allowing the rapid screening of many candidates. However, these assays lack physiological relevance. The latter compensates by offering the complexity of a living system. However, animal models lack human relevance.
A new branch of technologies, collectively called New Alternative Methods, or New Approach Methodologies (NAMs), aims to bridge the relevance gap by modeling the physiological processes of human organs and systems.
NAMs are any methodology, technology, approach, or combination that provides information on drug hazard and risk assessment while avoiding whole animal use. This includes in chemico, in silico, ex vivo, and in vitro methods. The beneficial role of NAMs in drug development and discovery has become more evident after the FDA's Modernization Act 2.0.
The “Alternatives to Animal Testing” bill has allowed the FDA to accept data derived from non-animal drug testing methods in IND submissions, where enhanced performance has been proven.
An introduction to Organ-on-a-chip
Over the past decade, Organ-on-a-chip (OOC) technology has gained traction within the NAM market. OOCs, or microphysiological systems (MPS), were originally described in 2010 with Harvard University’s lung-on-a-chip model, generated via microfluidic devices that supported academics with cell culture.1 This opened the door for the commercial development of several other organ models and technology providers.
OOC technologies generate 3D microtissues that recapitulate the functions, microarchitecture, and physiological responses of human organs and tissues with greater accuracy than conventional preclinical models.
3D microtissues are grown by co-culturing organ-specific primary human cells in the presence of microfluidic perfusion (to mimic the bloodstream), providing oxygen, biomechanical stimuli, nutrients, and waste removal.
OOC technology also allows for complex stimuli like growth factors to trigger cellular processes, interferons to stimulate an immune response, fat loading to imitate Western diets, and drug dosing to predict their human effects.
OOCs can be utilized at many drug discovery and development phases. When combined with existing methodologies (and additional NAMs), their human-relevant insights cross-validate, supplement, or query existing datasets, delivering a “larger picture” for more informed decision-making.
Independent research reports that 26 % of all research and development costs could be saved where OOCs are integrated into Pharma workflows.2 Market research supports this, underscoring the three best reasons for OOC purchase: to detect/recover flawed drugs, reduce costs, and improve the human translatability of results.
OOC applications across the preclinical landscape
In early discovery, OOC technology enables a deeper comprehension of human physiology and disease mechanisms to support target identification and validation. OOCs complement animal models, patient-derived clinical samples, and other in vitro preclinical tools by corroborating target-specific data or uncovering new roads to explore.
The same OOC models can be utilized in lead optimization to inform and complement in vivo efficacy studies by allowing a wider range of conditions to be investigated before expensive animal studies. When the effective therapeutic dose range is refined early, subsequent animal use can be minimized.
Throughout the drug discovery phase, OOCs can be adopted to generate toxicology profiles. Drug-induced liver injury (DILI) is a key contributor to late-stage drug failures and market withdrawal. However, it is possible to de-risk the process by incorporating liver-on-a-chip models into the preclinical toolbox.
With heightened performance compared to standard techniques, liver-on-a-chip provides a more sensitive method to discover potential adverse effects earlier in the process, allowing the recovery of promising, but flawed, drugs. 3
As development progresses, these predictive human models can be a companion to animal studies to query or confirm unexpected drug toxicity, efficacy, and Absorption, Distribution, Metabolism, and Excretion (ADME) results. OOC models lower the chance of false reporting resulting from interspecies issues. In specific cases, OOCs offer a direct alternative to animals - particularly for testing new modality drugs with human-specific targets where translatability to humans is weak.
Human-specific drug modalities (such as antibody, cell, and gene therapies) pose a notable challenge to development. Interspecies differences in metabolism, genetics, or immunological response can make animal models ill-suited for safety and efficacy testing when investigating advanced therapies. There are similar issues when predicting immune-mediated, or idiosyncratic toxicity.
OOC models can be designed to recapitulate elements of the human adaptive and innate immune response by incorporating tissue-specific immune cells and peripheral blood mononuclear cells (PBMCs) to increase assay sensitivity.
When adverse effects go undetected within discovery, and later come to light during clinical trials, OOCs can used to recreate the clinical scenario and help discover the cause.
OOC in the lab
OOC's adoption has been simplified, with a range of commercially available hardware, kits, consumables, and pre-validated primary cells. OOC models are also highly versatile, providing users with the ability to precisely modify the type and ratio of primary human cells to suit a wide array of contexts of use.
For example, simple primary human hepatocyte (PHH) monocultures can be used in isolation to overcome the limitations of standard drug metabolism assays to predict the human in vivo clearance rates of slowly metabolized drugs, or to identify rare or human-specific metabolites.4
To recapitulate human immune responses, duo-cultures of PHH and Kupffer cells enable researchers to investigate immune-mediated toxicity in DILI assays.5 The model can be enhanced further by adding circulating PBMCs into the flow that perfuses organs to flag idiosyncratic toxicity.6
To recreate common metabolic liver diseases like Metabolic dysfunction associated steatohepatitis (MASH), previously known as non-alcoholic steatohepatitis (NASH), a co-culture of PHH, Kupffer, and human stellate cells is grown to form a liver microtissue that is subsequently exposed to fat-loading, thereby triggering the disease state. In 2021, Kostrzewski et al. showed that the model accurately recapitulates vital aspects of the human condition.7
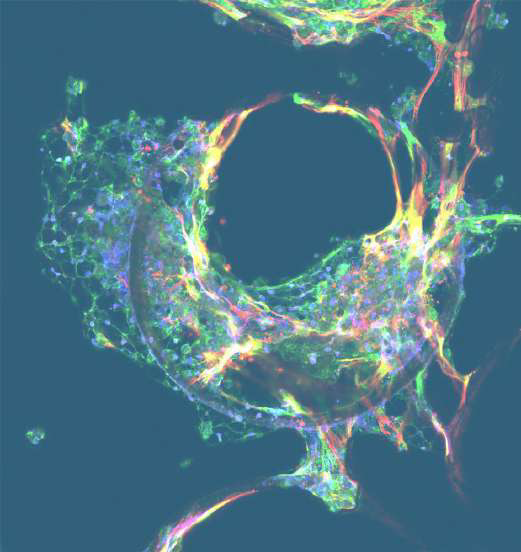
Image Credit: CN Bio
Vacca et al. utilized transcriptomic profiling to demonstrate that the model can more accurately replicate changes found in NASH patients compared to the conventional murine WD model.8 This predictive human model can also be used to identify increased DILI susceptibilities in patients diagnosed with the underlying disease to minimize the risk of drugs exacerbating the pre-existing condition.
Liver-on-a-chip tissues are functional, metabolically active, and available for experiments after four days of culture. Depending on the context of use, and dosing schedule, each liver chip can be investigated for two to four weeks.
For toxicity investigations, optimal results can be reached over eight to ten days. However, it may be beneficial to extend the period of disease modeling and efficacy studies to observe longer-term drug effects. These models provide a quicker, more human-relevant, and financially viable approach compared to animal models.
Numerous OOC models also allow for the periodic performance of imaging and/or sample recovery throughout experiments, providing high-content longitudinal data to measure responses like biomarker production, metabolite formation, or phenotypic responses.
OOC assay data is generated through standard laboratory methods like sequencing, microscopy, mass spectrometry, histology cytometry, and multiplexed immunoassays to produce deep insights from each sample.
High-profile groups, like the FDA, have released studies highlighting the robustness of OOC data. They confirm the reproducibility of drug response data at several test sites utilizing the PhysioMimix® system and the superior performance of this approach for toxicity, drug metabolism, and accumulation applications compared to in vivo animal models.3
Moving ahead of culturing single-organ models in isolation, it is now possible to interconnect OOC models into fluidically linked multi-organ systems. For example, the integration of liver models with lung or gut models recapitulates prevalent practices of drug administration.
Multi-organ systems simulate processes like drug absorption and first-pass metabolism to predict human drug bioavailability in vitro. Combined with physiologically based pharmacokinetic modeling, the data from OOCs can be extrapolated from an in vitro result into an in vivo prediction to inform dosing recommendations.
Multi-organ models also facilitate interorgan crosstalk for the evaluation of on- and off-target drug effects or to research inflammation and other risks when investigating drug effects.
A look to the future
OOCs represent a solid approach to refining, reducing, and complementing existing drug testing methodologies. Market research has shown that 66 % of respondents are currently utilizing or have plans to adopt OOC within two years.
This highlights that these technologies are poised to transform drug discovery and testing by enabling the in vitro recapitulation of human physiology. OOCs offer lower cost, higher throughput animal alternatives and can complement or replace as necessary.

Image Credit: CN Bio Innovations Limited
By improving data translatability between the clinic and the laboratory more accurate preclinical predictions (in terms of human responses) can be gleaned right now to decrease the risk of unforeseen failures during human clinical trials.
The routine use of OCC within drug discovery and development workflows is happening - it simply does a better job than traditional approaches. Smart investment in the technology alongside additional NAMs, including in silico modeling and artificial intelligence will potentially save countless hours and billions of research and development dollars.
References and further reading
- Huh D, et al. (2010) Reconstituting organ-level lung functions on a chip. Science. Jun 25;328(5986):1662-8. doi: 10.1126/ science.1188302. https://pubmed.ncbi.nlm.nih.gov/20576885/.
- Franzen et al (2019). Impact of organ-on-a-chip technology on pharmaceutical R&D costs. Drug Discov Today. 2019 Sep;24(9):1720-1724. doi: 10.1016/j.drudis.2019.06.003. Epub 2019 Jun 8. PMID: 31185290. https://pubmed.ncbi.nlm.nih.gov/31185290/
- Rubiano, A et al (2021). Characterizing the reproducibility in using a liver microphysiological system for assaying drug toxicity, metabolism, and accumulation.Clinical and Translational Science, 14(3), 1049-1061. https://doi.org/10.1111/cts.12969
- Docci L, et al (2022) . Exploration and application of a liver-on a-chip device in combination with modelling and simulation for quantitative drug metabolism studies. Lab Chip. 15;22(6):1187- 1205. doi: 10.1039/d1lc01161h. PMID: 35107462.)
- Novac, O et al. (2022). Human Liver Microphysiological System for Assessing Drug-Induced Liver Toxicity In Vitro. J. Vis. Exp. (179), e63389, doi:10.3791/63389 https://www.jove.com/t/63389/ human-liver-microphysiological-system-for-assessing-drug-induced
- https://cn-bio.com/, visited on 24 May 2023
- Kostrzewski T, et al. (2019). A Microphysiological System for Studying Nonalcoholic Steatohepatitis. Hepatol Commun. Nov 13;4(1):77-91. doi: 10.1002/hep4.1450. PMID: 31909357; PMCID: PMC6939502. https://pubmed.ncbi.nlm.nih.gov/31909357/
- Vacca, M, et al (2020). Bone morphogenetic protein 8B promotes the progression of non-alcoholic steatohepatitis. Nat Metab 2, 514–531 https://doi.org/10.1038/s42255-020-0214-9
About CN Bio
CN Bio is a leading organ-on-a-chip (OOC) company that offers a portfolio of products and contract research services to optimize the accuracy and efficiency of bringing new medicines to market. With more than a decade of research and development experience, they aim to transform the way human-relevant pre-clinical data is generated through the development of advanced in vitro human organ models.
CN-Bio's PhysioMimix® Core microphysiological system (MPS) enables researchers to recreate human biology in the lab and is the only microphysiological system with validated performance across single-, multi-organ, and higher throughput configurations. This easy to adopt, adapt and scale technology bridges the gap between traditional cell culture and human studies, to support the development of safer and more efficacious therapeutics, whilst reducing the dependence on animal model usage.
CN Bio’s portfolio of products (MPS, 3D validated cells, consumable plates) and services support researchers that require reliable, data-rich, in vitro studies, to uncover novel mechanistic insights into drug or disease mechanism of action.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.