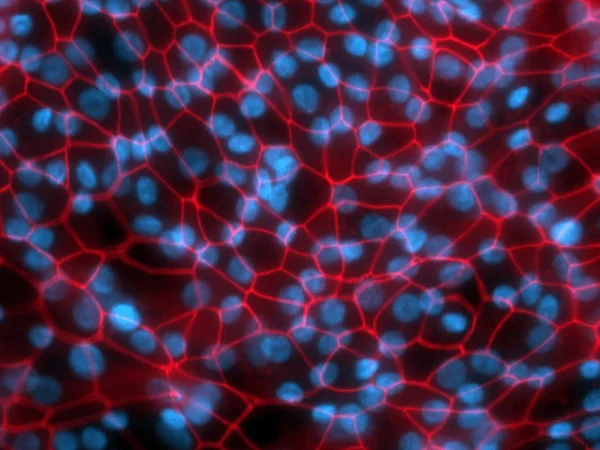
Small Airway Epithelial Cells immunostained to detect junctional protein ZO1, a marker for tight junctions. Image Credit: Newcells Biotech
Lung toxicity and fibrosis are caused by inhaling particles, pathogens, and therapeutics. They can also occur following repeated administration of systemic and oral drugs.
Any epithelial damage or loss of epithelial barrier integrity triggers an immune response that results in inflammation, tissue damage, and potentially lung toxicity. This increases vulnerability to infection and impairs gas exchange.
In vitro epithelial cell culture models, like Newcells' small airway epithelial cell (SAEC) model, evaluate several epithelial damage parameters to provide predictive data that allows precise predictions of treatments' possible cellular toxicity.
Service outputs
- MTT activity
- TEER
- LDH release assay
- ATP activity quantification
Assays
- LDH release
- ATP assay
- MTT assay
- TEER
Models
- Human small airway epithelial cells on air-liquid interface (ALI) (24 well)
Timeline
How to access the lung toxicity assay service
Newcells has over ten years of experience in lung research and can assist users in creating experiments that suit their requirements.
Service overview
The fully differentiated, polarized human SAEC model, cultured on 3D permeable supports, enables the addition of xenobiotics to either the apical or basolateral compartments to assess their effects on the integrity of the epithelial barrier and whether they cause the release of cytokines in response to cell damage.
To assess drug-induced lung toxicity, Newcells typically measures four assay readouts. TEER, LDH release, and ATP/MTT activity all show a dose-dependent response to the antibiotic puromycin, which has toxic side effects in the lungs.
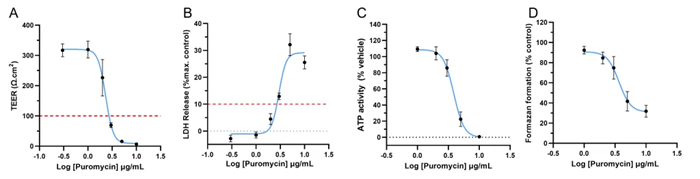
Puromycin induces a dose-dependent response as measured by A) TEER, B) LDH release, C) cellular ATP activity, and D) formazan formation. After stimulating Newcells’ SAEC-ALI model with specified concentrations of Puromycin for 72 hours, resultant cell and epithelium damage show a dose-dependent decrease in TEER, associated with increased LDH release. Data shows a dose-dependent reduction in ATP activity and cell viability. Image Credit: Newcells Biotech
Source: Newcells Biotech
| |
| Models |
Primary small airway epithelial cell model with an ALI (air-liquid interface).
The model includes all major cell types of the lung epithelium:
- Basal cells
- Club cells
- Goblet cells
- Ciliated cells
|
| Assay format |
24-well |
| Species |
Human |
| Assay readout |
TEER |
| Cell viability (LDH, ATP, MTT) |
| Biological variation |
3 human healthy donors (recommended) |
| Technical replicates |
3 technical replicates per condition (recommended) |
| Assay treatment window |
72 hours |