The ongoing coronavirus disease 2019 (COVID-19) pandemic caused by SARS-CoV-2 has put a lot of burden on the healthcare systems of many countries across the world. Although SARS-CoV-2 primarily spreads from person to person via respiratory droplets, there is evidence suggesting the possibility of airborne transmission. The spike protein on the viral surface interacts with the host angiotensin-converting enzyme 2 (ACE2) receptor to enter the respiratory epithelial cells. With an incubation period of 2 to 14 days, SARS-CoV-2 generally induces mild or no symptoms in about 80% of infected individuals.
Polymerase chain reaction (PCR)-based detection of viral RNA is considered to be the most accurate procedure to diagnose an active SARS-CoV-2 infection. However, detection of SARS-CoV-2 specific antibodies in the blood (through antibody tests) is vital for identifying past infection that has probably induced adaptive immune responses in individuals who remained asymptomatic or mildly symptomatic during the active infection phase. However, it is still uncertain how many COVID-19 recovered individuals develop antibodies, how long the antibodies remain active, and if antibodies can provide protection against reinfection.
Because front-line workers – such as healthcare personnel, police, and firefighters – are at a relatively higher risk of getting SARS-CoV-2 infection, the current study’s scientists aimed at determining the prevalence of SARS-CoV-2 specific IgG antibodies among front-line personnel working in Lubbock, Taxus, and nearby regions.
Current study design
A total of 683 asymptomatic workers (age range: 18 – 76 years) were enrolled for the study. FDA-approved commercially available antibody detection kits were used to measure the anti- SARS-CoV-2 antibody levels in the blood.
Important observation
Of all participants, only five tested positive for anti-SARS-CoV-2 IgG antibodies. Gender-wise, two of IgG-positive participants were females, and three were males; occupation-wise, two were firefighters, two were police officers, and one was an emergency medical technician. Of the five IgG-positive participants, only the medical technician reported having medically diagnosed COVID-19 with mild symptoms 2 months before the study period. The rest of them did not report having known SARS-CoV-2 infection or known exposure to COVID-19 patients previously.
A significant portion of the participants who tested negative in the antibody test reported having COVID-19 related symptoms (fever, cough, and breathlessness) within the last 5 months. However, none of them tested positive for SARS-CoV-2. About 50% of participants reported exposures to known COVID-19 cases. However, they were properly protected by personal protective equipment (PPE) during the exposures.
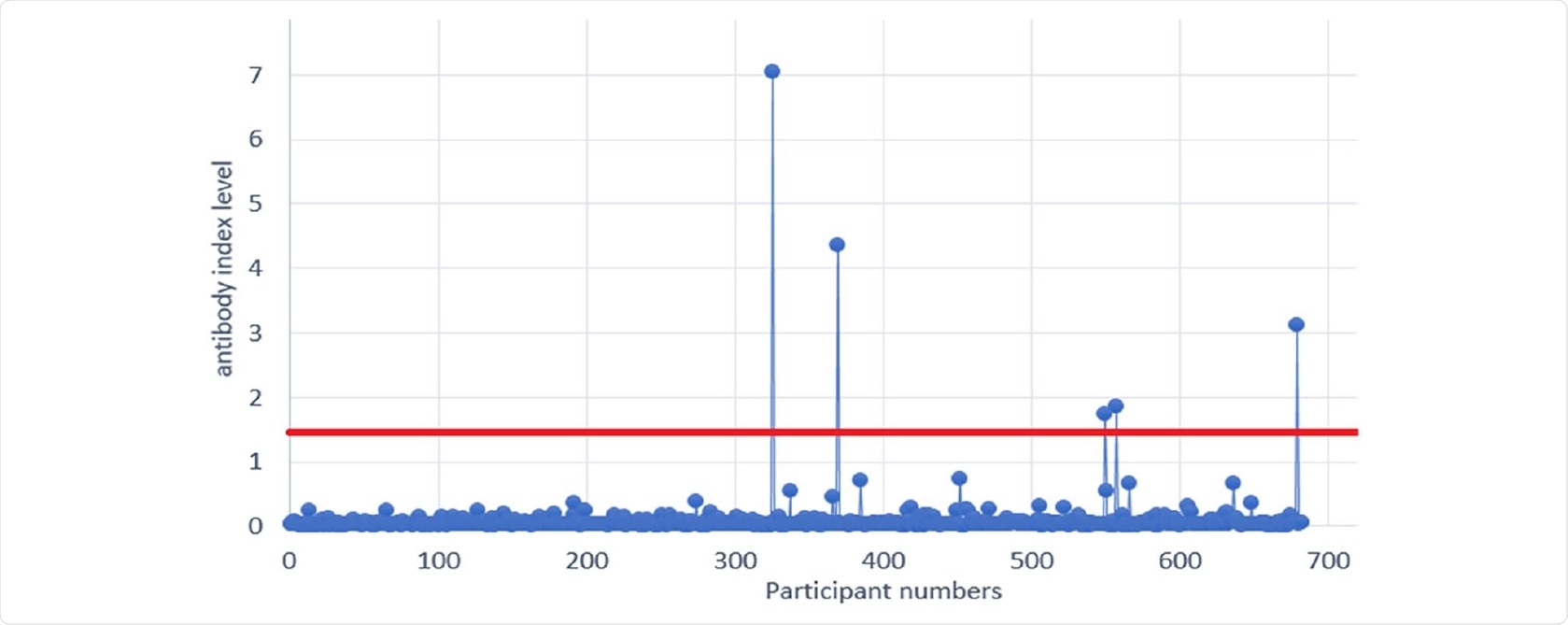
SARS-CoV-2 antibody levels among first responders (vertical axis - participant numbers. Horizontal axis - SARS-CoV-2 antibody level measured in index. Positive threshold is 1.4 index and above).
Study significance
Although the risk of viral transmission is expected to be higher among front-line workers, the current study findings surprisingly reveal that the prevalence of anti-SARS-CoV-2 IgG antibodies in front-line workers is less than 1%. This indicates that different safety measures, including PPE, are properly implemented in workplaces in Lubbock county and nearby regions.
According to the scientists, many factors might be responsible for this lower than expected antibody prevalence. For example, the duration between viral exposure and the development of IgG response is vital for antibody detection. An antibody test conducted too early can lead to negative results. It is also possible that IgG antibodies developed in response to SARS-CoV-2 do not persist for a long time. There is evidence suggesting that the level of anti-SARS-CoV-2 antibody starts declining within 2 months.
Another possibility is that the IgA-mediated immune response in the respiratory tract, which develops earlier than the IgG-mediated response, is sufficient to eliminate the virus. This is particularly true for mild SARS-CoV-2 infection. Because of the early elimination, the virus does not get a chance to enter the blood and trigger the production of IgG antibodies.
Compared to other cities in the US, the significantly lower prevalence of SARS-CoV-2 infection in the general population in Lubbock county may be attributed to the lower antibody prevalence.
Taken together, the scientists believe that the low antibody prevalence observed in the current study signifies the efficacy of current PPE measures. Thus, a low infection rate can be maintained among front-line workers by strictly implementing appropriate control measures.